
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.

Chapter 6: CONNECTIVE TISSUE
Introduction.
Chapter Objectives
After studying this chapter, you will be able to:
- Identify and describe the general organisation of the cells and intercellular substances of connective tissue
- Classify connective tissue subtypes
- Examine the macroscopic and microscopic appearance of a range of connective tissue types
Connective tissue is the most widely distributed primary tissue in the human body. As may be obvious from its name, one of the major functions of connective tissue is to support and connect tissues and organs. Unlike epithelial tissue, which is composed of cells closely packed with little or no extracellular space in-between, connective tissue cells are dispersed in a matrix. The matrix usually includes a large amount of extracellular material produced by the connective tissue cells that are embedded within it. The matrix plays a major role in the functioning of this tissue. The major component of the matrix is a ground substance often crisscrossed by fibres. This ground substance is usually a fluid, but it can also be mineralised and solid, as in bones. Connective tissues come in a vast variety of forms, yet they typically have in common three characteristic components: cells, large amounts of amorphous ground substance, and fibres. The amount and structure of each component correlates with the function of the tissue, from the rigid ground substance in bones supporting the body to the housing of specialised cells, for example, a phagocytic cell that engulfs pathogens and also rids tissue of cellular debris.
General Features of Connective Tissues
Learning Objectives
By the end of this section, you will be able to:
- Describe the types of connective tissue: proper, supportive, and fluid
- Identify and describe the major cell types found in connective tissue proper
- Describe the intercellular substances in connective tissues including fibres and amorphous ground substance
Connective tissues are characterised by their abundance of intercellular material and relatively few cells. The intercellular material or matrix consists of a range of connective tissue fibres and amorphous ground substances. The three broad categories of connective tissue are classified according to the characteristics of their ground substance and the types of fibres found within the matrix ( Table 4.1 ). Connective tissue proper (or general connective tissue) includes loose connective tissue and dense connective tissue . Both tissues have a variety of cell types and protein fibres suspended in a viscous ground substance. Dense connective tissue is reinforced by bundles of fibres that provide tensile strength, elasticity and protection. In loose connective tissue, the fibres are loosely organised, leaving large spaces in between.
Supportive connective tissue —bone and cartilage—provide structure and strength to the body and protect soft tissues. A few distinct cell types and densely packed fibres in a matrix characterise these tissues. In bone, the matrix is rigid and described as calcified because of the deposited calcium salts. In fluid connective tissue , in other words, lymph and blood, various specialised cells circulate in a watery fluid containing salts, nutrients, and dissolved proteins. Supportive and fluid connective tissues are collectively referred to as specialised connective tissues .
Table 4.1 Connective Tissue Examples
Fibroblasts and adipocytes cells are fixed cells, which means they remain within the connective tissue. Other cells (migratory or wandering cells) move in and out of the connective tissue in response to chemical signals. Macrophages, leucocytes and phagocytic cells are found in connective tissue proper but are actually part of the immune system protecting the body ( Figure 4.9 ). The most abundant cell present in all subtypes of connective tissue proper is the fibroblast . Fibroblasts are spindle-shaped with moderate amounts of cytoplasm and a large oval nucleus when active. In their inactive or resting form, fibroblasts have reduced cytoplasm and small, flattened and elongated nuclei. Polysaccharides and proteins secreted by fibroblasts combine with extra-cellular fluids to produce a viscous ground substance that, with embedded fibrous proteins, forms the extra-cellular matrix.
Adipocytes are cells that store lipids as droplets that fill most of the cytoplasm. The number and type of adipocytes depends on the tissue and location, and vary among individuals in the population. Adipocytes can be recognised by the large lipid droplet that occupies the majority of the cell and pushes the nucleus to the periphery of the cell in an eccentric and flattened position. They appear as large white circular cells in stained sections ( Figure 4.9 ).
The macrophage is a large cell derived from a monocyte, a type of leukocyte found in the blood, which enters the connective tissue matrix from the blood vessels. Roaming, or free, macrophages move rapidly through the intercellular matrix, engulfing infectious agents and cellular debris. Connective tissues also house fixed macrophages that are permanent residents of their tissues. The appearance of macrophages is highly variable due to the range of subtypes and depending on its funcitonal state (active or resting). Similar to macrophages, wandering leucocytes such as lymphocytes can also enter connective tissue proper to perform lymphatic functions including phagocytosis, allergic or inflammatory reactions and immune defence. Lymphocytes can be recognised by their large round nucleus that occupies almost all of the cytoplasm of the cell.
Mesenchymal stem cells are also commonly found in connective tissues where they can differentiate into a range of mature cell types such as adipocytes, fibroblasts and specialised connective tissue cells including bone and cartilaginous cells.
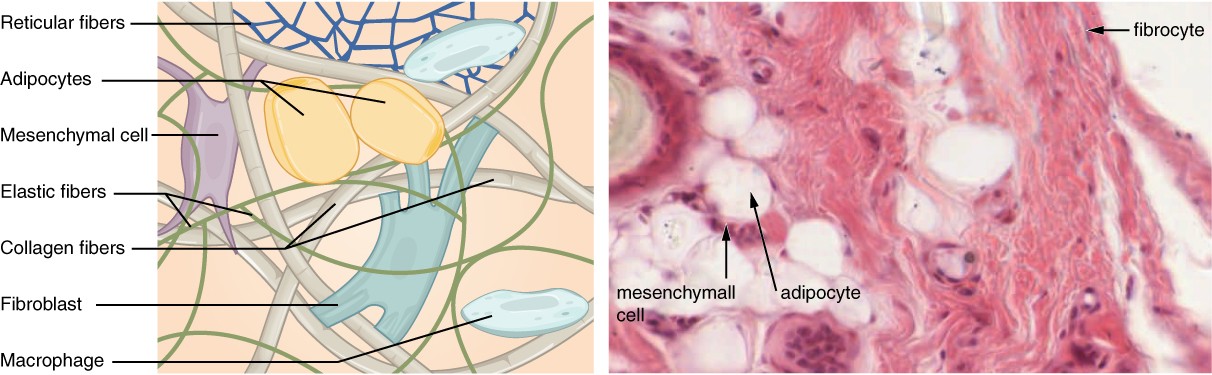
Figure 4.9 Connective Tissue Proper Fibroblasts produce the extracellular matrix of this connective tissue. Connective tissue proper includes the fixed cells fibrocytes, adipocytes, and mesenchymal cells. Migratory cells such as macrophages can enter connective tissues when needed. LM × 400. [Micrograph provided by the Regents of University of Michigan Medical School © 2012]
Connective Tissue Fibres and Ground Substance
Intercellular substances are the predominant components of most types of connective tissue (adipose tissue being the exception). There are two types of intercellular substances, amorphous ground substances and fibres. Three main types of fibres are secreted by fibroblasts: collagenous fibres, reticular fibres and elastic fibres.
All of these fibre types and connective tissue cells are embedded in amorphous ground substance . Secreted by fibroblasts, ground substance is made of carbohydrates and proteins. Amorphous ground substance appears as clear spaces between the fibres and cells of a connective tissue in typical histological preparations as they usually dissolve out of the tissue section during preparation.
Connective Tissue Proper
- Identify and describe the microscopic features of loose and dense connective tissue subtypes: areolar, adipose, reticular, dense regular and dense irregular connective tissue
- Describe common locations for each of the connective tissue proper subtypes
Connective tissue proper or general connective tissues can be classified into two major types based on the density of connective tissue fibres. A connective tissue that is characterised microscopically by a relative abundance of cells and ground substance and a loose arrangement of fibres is referred to as loose connective tissue. Dense connective tissues are distinguished microscopically by the close packing of their fibres and relatively few cells and little ground substance.
Loose Connective Tissue
Loose connective tissue is found between many organs where it acts both to absorb shock and bind tissues together. It allows water, salts and various nutrients to diffuse through to adjacent or embedded cells and tissues. There are three types of loose connective tissue: areolar adipose and reticular connective tissue.
Areolar tissue is the most common form of loose connective tissue and shows little specialisation. It contains all the cell types and fibres previously described and is distributed in a random, web-like fashion. It occupies the superficial fascia (hypodermis of skin), fills the spaces between muscle fibres, surrounds blood and lymph vessels, and supports organs in the abdominal cavity. Areolar tissue underlies most epithelia and represents the connective tissue component of epithelial membranes.
INTERACTIVE ACTIVITY
Adipose tissue consists mostly of adipocytes, with little extracellular matrix ( Figure 4.10 ). A large number of capillaries are also present to allow rapid storage and mobilisation of lipid molecules.
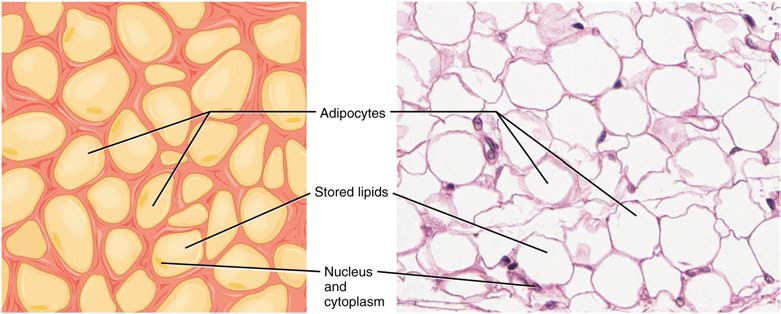
Figure 4.10 Adipose Tissue This is a loose connective tissue that consists of fat cells with little extracellular matrix. It stores fat for energy and provides insulation. LM × 800. [Micrograph provided by the Regents of University of Michigan Medical School © 2012]
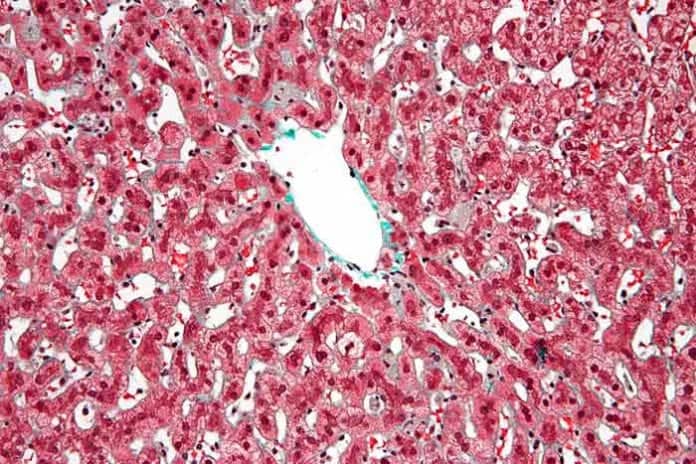
Reticular tissue is a mesh-like, supportive framework for soft organs such as lymphatic tissue, the spleen and the liver ( Figure 4.11 ). Fibroblasts produce the reticular fibres that form the network onto which other cells attach. It derives its name from the Latin reticulus , which means “little net.”
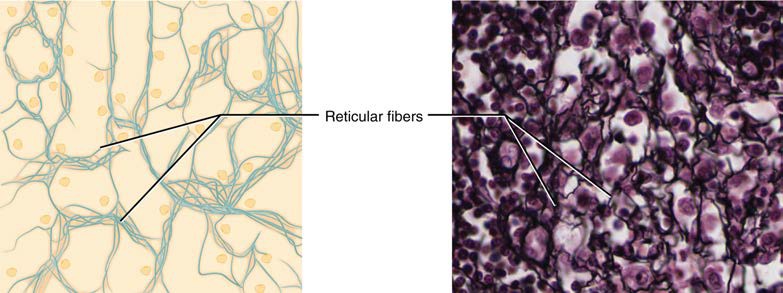
Figure 4.11 Reticular Tissue This is a loose connective tissue made up of a network of reticular fibres that provides a supportive framework for soft organs. Note the black staining of the densely branching reticular fibres. LM × 1600. [Micrograph provided by the Regents of University of Michigan Medical School © 2012]
Dense Connective Tissue
Dense connective tissue contains more collagenous fibres than does loose connective tissue. As a consequence, it displays greater resistance to stretching. There are two major categories of dense connective tissue: regular and irregular. Dense regular connective tissue fibres are parallel to each other, enhancing tensile strength and resistance to stretching in the direction of the fibre orientation. Ligaments and tendons are made of dense regular connective tissue, but in ligaments not all fibres are parallel. Whilst collagenous fibres are the most abundant fibre type in structures composed of dense regular connective tissue, elastic fibres are also found in some examples and in different proportions. For example ligaments have a relatively higher proportion of elastic fibres than is seen in tendons, bestowing different physical properties to each of these structures. In photomicrographs the collagenous fibres appear wavy due to the natural protein arrangement of collagen. This ‘crimping’ straightens out with the tissue is placed under tension.
In dense irregular connective tissue , the direction of fibres is random. This arrangement gives the tissue greater strength in all directions and less strength in one particular direction. In some tissues, fibres crisscross and form a mesh. In other tissues, stretching in several directions is achieved by alternating layers where fibres run in the same orientation in each layer, and it is the layers themselves that are stacked at an angle. The dermis of the skin, fibrous capsules of some organs, the periosteum and endosteum and deep fascia are examples of dense irregular connective tissue rich in collagenous fibres ( Figure 4.12 ). Note the appearance of the bundles of collagenous fibres in dense irregular connective tissue in photomicrographs are cut in cross-section as well as running longitudinally due to the irregular organisation of fibres.
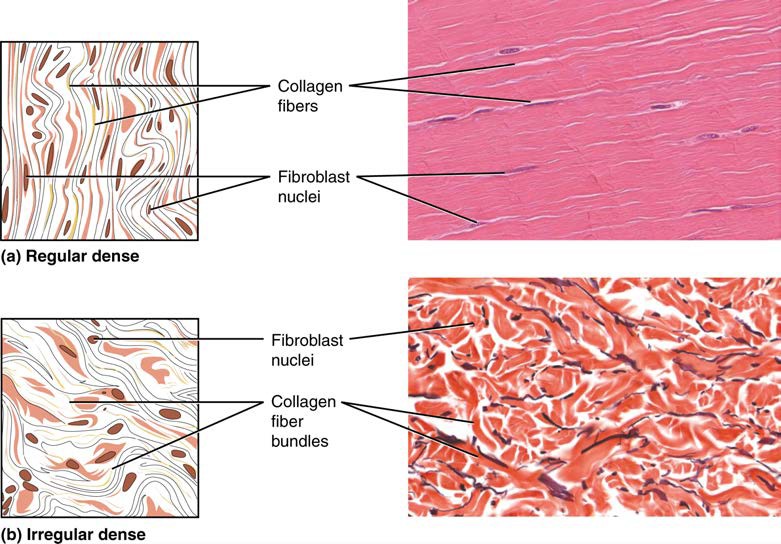
Figure 4.12 Dense Connective Tissue (a) Dense regular connective tissue consists of collagenous fibres packed into parallel bundles. (b) Dense irregular connective tissue consists of collagenous fibres interwoven into a mesh-like network. From top, LM × 1000, LM × 200. [Micrographs provided by the Regents of University of Michigan Medical School © 2012]
Specialised Connective Tissues
- Identify and describe the microscopic features of cartilaginous tissue subtypes: hyaline, elastic and fibrous cartilaginous tissue
- Identify and describe the microscopic features of bone tissue subtypes: cortical and trabecular bone tissue
- Describe common locations for each of the specialised connective tissue subtypes
Specialised connective tissues include supportive and fluid connective tissues. Two major forms of supportive connective tissue, cartilage and bone, allow the body to maintain its posture and protect internal organs.
Cartilaginous Tissue
The distinctive appearance of cartilaginous tissue is due to carbohydrates, which bind with ground substance proteins. Embedded within the cartilage matrix are chondrocytes , or cartilage cells, and the space they occupy in the semisolid matrix are called lacunae (singular = lacuna). Cartilaginous tissue is avascular, thus all nutrients need to diffuse through the matrix to reach the chondrocytes. This is a factor contributing to the very slow healing of cartilaginous tissues. The three main types of cartilaginous tissue are hyaline cartilage, fibrocartilage, and elastic cartilage ( Figure 4.13 ).
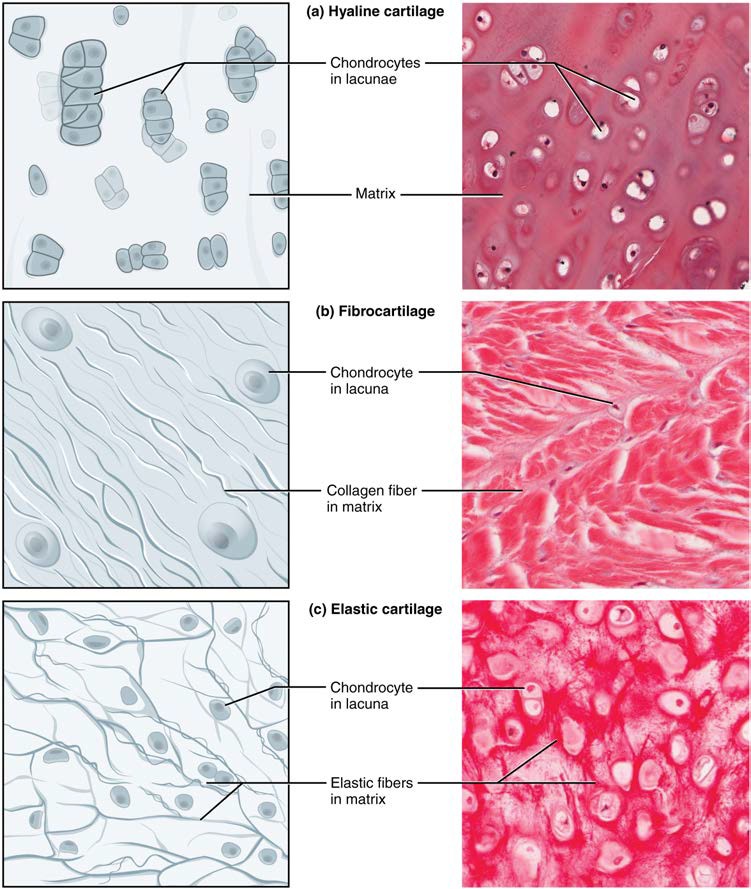
Figure 4.13 Types of Cartilaginous tissue Cartilaginous tissue is a supportive connective tissue consisting of collagenous fibres embedded in a firm matrix of chondroitin sulfates. (a) Hyaline cartilaginous tissue provides support with some flexibility. Fibres are difficult to visualise in typical stained sections as they are so small. (b) Fibrocartilage provides some compressibility and can absorb pressure. (c) Elastic cartilage provides firm but elastic support. Note the chondrocytes in lacunae in all cartilaginous tissue subtypes. From top, LM × 300, LM × 1200, LM × 1016. [Micrographs provided by the Regents of University of Michigan Medical School © 2012]
Bone Tissue
Bone tissue is a highly vascular mineralised form of connective tissue. It is the only connective tissue subtype with a biphasic composition have an organic phase (fibres, amorphous ground substance and cells) making up on third of bone tissue and an inorganic phase (minerals) making up the remaining two thirds of bone tissue. It provides protection to internal organs and supports the body. Bone tissue also as important functions in calcium homeostasis and acts as a primary location for blood cell production (haematopoesis) within the bone marrow compartment. Bone’s rigid extracellular matrix contains mostly collagenous fibres embedded in a mineralised ground substance. The combination of having both organic and inorganic phases makes bone hard and flexible at the same time. Without the organic phase, bones would be brittle and shatter easily. Without mineral crystals, bones would flex and provide little support. Unlike cartilage, bone tissue can recover from injuries in a relatively short time due to its highly vascular composition.
Bone contains a relatively small number of cells entrenched in a matrix of collagenous fibres that provide a surface for inorganic salt crystals to adhere. These salt crystals form when calcium phosphate and calcium carbonate combine to create hydroxyapatite, which incorporates other inorganic salts like magnesium hydroxide, fluoride, and sulfate as it crystallises, or calcifies, on the collagenous fibers.
Although bone cells compose a small amount of the bone volume, they are crucial to the function of bones. Four types of cells are found within bone tissue: osteoblasts, osteocytes, osteogenic cells , and osteoclasts ( Figure 6.11 ).
The osteoblast is the bone cell responsible for forming new bone tissue and is found on bone surfaces within the periosteum and endosteum (dense irregular connective tissue membranes that line bone surfaces). Osteoblasts are cuboidal-shaped cells, do not divide, and are responsible for the synthesis and secretion of the collagenous matrix (or osteoid ). As the secreted matrix surrounding the osteoblast calcifies, the osteoblast becomes trapped within it; as a result, it changes in structure and becomes an osteocyte , the primary cell of mature bone and the most common type of bone cell. Each osteocyte has a round body with multiple cytoplasmic processes that radiate out from the body. They are located in a space called a lacuna (plural = lacunae) and are surrounded by bone tissue. Osteocytes have an important role in survellance of the bone tissue to maintain bone strength including stimulating bone repair at sites of bone weakness or damage, and detecting mechanical signals from the external environment in response to exercise. In this way, osteocytes have an essential role in maintaining the strength of bone tissue and dynamically adapting to the loads placed on our bodies. Like osteoblasts, osteocytes lack mitotic activity. They can communicate with each other and receive nutrients via their long cytoplasmic processes that extend through canaliculi (singular = canaliculus), channels within the bone matrix.
If osteoblasts and osteocytes are incapable of mitosis, then how are they replenished when old ones die? The answer lies in the properties of a third category of bone cells —the osteogenic cell . These osteogenic cells are undifferentiated with high mitotic activity and they are the only bone cells that divide. Immature osteogenic cells are found in the deep layers of the periosteum and the bone marrow. They have the ability to differentiate and develop into osteoblasts.
The dynamic nature of bone means that new tissue is constantly formed, and old, injured, or unnecessary bone is dissolved for repair or for calcium release. The cell responsible for bone resorption , or breakdown, is the osteoclast . Osteoclasts are found on bone surfaces, are multinucleated, and originate from the function of multiple monocytes and not from osteogenic cells . Osteoclasts are continually breaking down old bone while osteoblasts are continually forming new bone . The process is known as bone remodelling . The ongoing balance between osteoblasts and osteoclasts is responsible for continuous release of calcium into the bloodstream to maintain calcium homeostasis, as well as to repair areas of bone damage and adapt to changes in the mechanical environment. Table 6.3 reviews the bone cells , their functions and locations.
Photomicrograph of Bone Tissue (Haemotoxylin and Eosin stain; x200 magnification) . Learn to accurately identify the three active bone cell types by clicking on each information hotspot in this histological section of trabecular bone tissue. [www.BEST.edu.au]
(a) Why do osteoclasts have multiple nuclei?
Bone Tissue Subtypes
Bones contain two types of bone tissue. Trabecular bone looks like a sponge under the microscope and contains empty spaces between trabeculae, or ‘little beams’ of bone tissue. It is lighter than cortical bone and found in the interior of some bones and at the end of long bones. Cortical bone is solid and has greater structural strength. The differences between cortical and trabecular bone are best explored via their histology. Most bones contain a combination of cortical and trabecular bone tissue, but their distribution and concentration vary based on the bone’s overall function. Cortical bone is dense so that it can withstand compressive forces, while trabecular bone has open spaces and supports loading from multiple directions.
Cortical Bone Tissue
Cortical bone, also known as compact or dense bone, is the denser, stronger of the two types of bone tissue ( Figure 6.12 ). It can be found forming the outer shell (cortex) of all bone organs and contains no macroscopic cavities. A higher proportion of cortical bone tissue can be observed in the diaphyses (shaft) of long bones, where it provides support and protection. The microscopic structural unit of cortical bone is called an osteon , or Haversian system. Each osteon is composed of concentric rings of calcified matrix called lamellae (singular = lamella). Running down the centre of each osteon is the central canal , or Haversian canal, which contains blood vessels, nerves and lymphatic vessels. These vessels and nerves branch off at right angles through a perforating canal , also known as Volkmann’s canals, to extend deeper within the cortical bone to connect the periosteum to the endosteum.
The osteocytes are located inside spaces called lacunae (singular = lacuna), found at the borders of adjacent lamellae. As described earlier, canaliculi connect lacunae and eventually with the central canal. This system allows nutrients to be transported to the osteocytes and wastes to be removed from them, as well as allowing the cytoplasmic processes of adjacent osteocytes to communicate with each other.
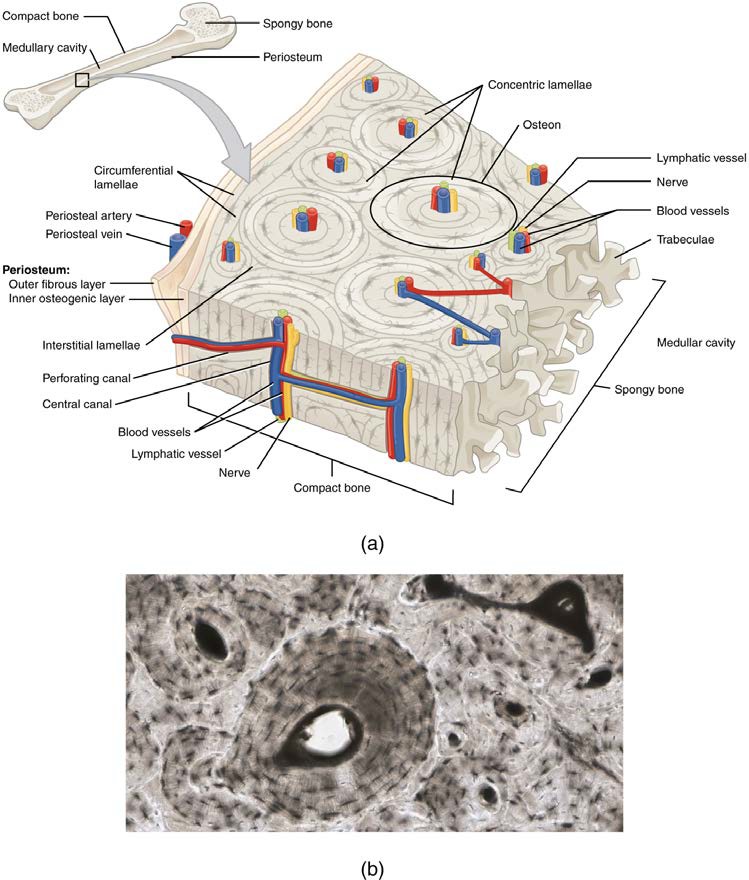
Figure 6.12 Diagram of Cortical Bone Tissue (a) This cross-sectional view of compact bone shows the basic structural unit, the osteon. (b) In this micrograph of the osteon, you can clearly see the concentric lamellae and central canals. LM × 40. [Micrograph provided by the Regents of University of Michigan Medical School © 2012]
Photomicrograph of Cortical Bone Tissue (Ground human bone, unstained; x200 magnification) . Learn to accurately identify the main features of cortical bone tissue by clicking on each information hotspot. [Berkshire Community College Bioscience Image Library]
(a) What is the purpose of lacunae and canaliculi?
(b) What is the structural unit of cortical bone tissue called?
Trabecular Bone Tissue
Like cortical bone, trabecular bone , also known as spongy or cancellous bone, contains osteocytes housed in lacunae, but they are not arranged in concentric circles. Instead, the lacunae and osteocytes are found in a lattice-like network of beams called trabeculae (singular = trabecula) ( Figure 6.13 ). The trabeculae may appear to be a random network, but each trabecula forms along lines of stress to provide strength to the bone. The spaces of the trabeculated network provide balance to the dense and heavy cortical bone tissue by making bones lighter so that muscles can move them more easily. In addition, the spaces in some trabecular bone tissue contain red bone marrow, where haematopoiesis occurs. A higher proportion of trabecular bone tissue is located in the ends of long bones (epiphyses and metaphyses) than cortical bone tissue, where the structural arrangement of trabecular bone tissue supports the multiple directions of loading experienced at the joint sites.
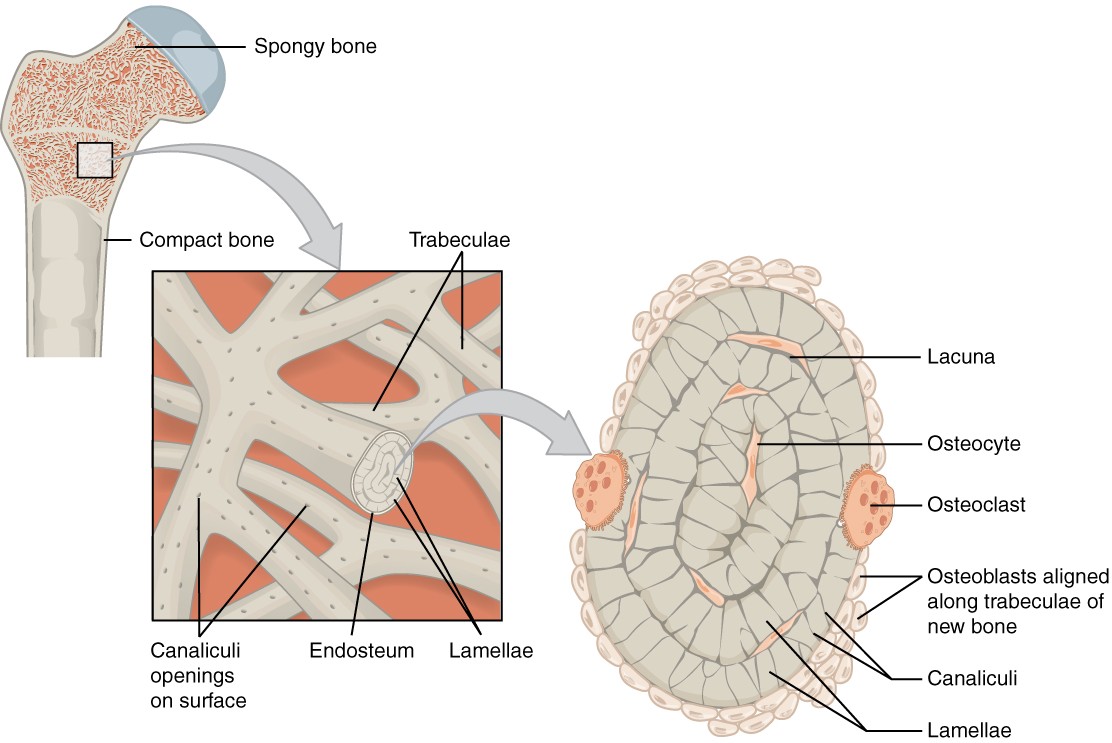
Figure 6.13 Diagram of Trabecular Bone Tissue Trabecular bone is composed of trabeculae that contain osteocytes in lacunae. Red bone marrow fills the spaces in some bones.
Photomicrograph of Trabecular Bone Tissue (Van Giesson and Haemotoxylin stain; x200 magnification) . Learn to accurately identify the main features of trabecular bone tissue by clicking on each information hotspot. [Mouse tissue; Attribution to Dr Laura Gregory, Queensland University of Technology]
Fluid Connective Tissue
Blood and lymph are fluid connective tissues. Cells circulate in a liquid extracellular matrix containing nutrients, salts and wastes. More information regarding fluid connective tissues can be found in the cardiovascular system chapter (blood) and the lymphatic system chapter (lymph).
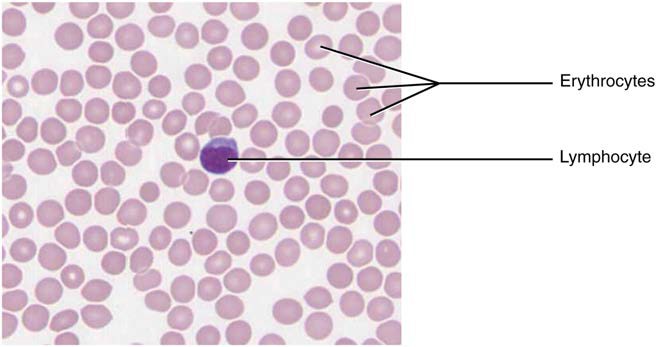
Figure 4.14 Blood: A Fluid Connective Tissue Blood is a fluid connective tissue containing erythrocytes and various types of leukocytes that circulate in a liquid extracellular matrix. LM × 1600. [Micrograph provided by the Regents of University of Michigan Medical School © 2012]
adipocytes lipid storage cells
adipose tissue specialised areolar tissue rich in stored fat
areolar tissue a type of connective tissue proper that shows little specialisation with cells dispersed in the matrix
cartilage semi-rigid connective tissue found on the skeleton in areas where flexibility and smooth surfaces support movement
canaliculi (singular = caniculus) channels within the bone matrix that house one of an osteocyte’s many cytoplasmic extensions that it uses to communicate and receive nutrients
central canal longitudinal channel in the centre of each osteon; contains blood vessels, nerves and lymphatic vessels; also known as the Haversian canal
chondrocytes cells of the cartilage
collagenous fibre flexible fibrous proteins that give connective tissue tensile strength
connective tissue type of tissue that serves to hold in place, connect, and integrate the body’s organs and systems
connective tissue proper connective tissue containing a viscous matrix, fibres, and cells
cortical bone tissue dense osseous tissue that can withstand compressive forces
dense connective tissue connective tissue proper that contains many fibres that provide both elasticity and protection
elastic cartilaginous tissue type of cartilaginous tissue, with elastin as the major protein, characterised by rigid support as well as elasticity
elastic fibre fibrous protein within connective tissue that contains a high percentage of the protein elastin that allows the fibres to stretch and return to original size
endosteum delicate membrane composed of dense irregular connective tissue lining the medullary cavity and trabeculae of a bone
fibroblast most abundant cell type in connective tissue, secretes protein fibres and matrix into the extracellular space
fibrocartilage tough form of cartilage, made of thick bundles of collagen fibers embedded in chondroitin sulfate ground substance
fluid connective tissue specialised cells that circulate in a watery fluid containing salts, nutrients, and dissolved proteins
ground substance fluid or semi-fluid portion of the matrix
hyaline cartilaginous tissue most common type of cartilaginous tissue, smooth and made of short collagenous fibres embedded in a chondroitin sulfate ground substance
lacunae (singular = lacuna) small spaces in bone or cartilage tissue that cells occupy
loose connective tissue type of connective tissue proper that shows little specialization with cells dispersed in the matrix
matrix extracellular material which is produced by the cells embedded in it, containing ground substance and fibres
mesenchymal cell adult stem cell from which most connective tissue cells are derived
mesenchyme embryonic tissue from which connective tissue cells derive
osteoblast cell responsible for forming new bone (organic bone matrix, osteoid)
osteoclast cell responsible for resorbing bone
osteocyte mature form of osteoblast that becomes surrounded by osteoid during bone formation; responsible for maintaining the matrix
osteogenic cell undifferentiated cell with high mitotic activity; the only bone cells that divide; they differentiate and develop into osteoblasts
osteoid uncalcified organic bone matrix secreted by osteoblasts
osteon (also, Haversian system) basic structural unit of cortical bone tissue; made of concentric layers (lamellae) of calcified matrix
perforating canal (also, Volkmann’s canal) channel that branches off from the central canal and houses vessels and nerves that extend to the periosteum and endosteum
periosteum dense irregular connective tissue membrane that covers the outer surface of bone tissue and is continuous with ligaments
reticular fibre fine fibrous protein, made of collagen subunits, which cross-link to form supporting “nets” within connective tissue
reticular tissue type of loose connective tissue that provides a supportive framework to soft organs, such as lymphatic tissue, spleen, and the liver
supportive connective tissue type of connective tissue that provides strength to the body and protects soft tissue; includes bone and cartilaginous tissues
trabecular bone tissue (also, spongy bone tissue) trabeculated osseous tissue that supports shifts in weight distribution
Human Anatomy (MASTER) Copyright © 2020 by Queensland University of Technology is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
Section 2: The Tissue Level of Organization
Connective tissue supports and protects.
As may be obvious from its name, one of the major functions of connective tissue is to connect tissues and organs. Unlike epithelial tissue, which is composed of cells closely packed with little or no extracellular space in between, connective tissue cells are dispersed in a matrix . The matrix usually includes a large amount of extracellular material produced by the connective tissue cells that are embedded within it. The matrix plays a major role in the functioning of this tissue. The major component of the matrix is a ground substance often crisscrossed by protein fibers. This ground substance is usually a fluid, but it can also be mineralized and solid, as in bones. Connective tissues come in a vast variety of forms, yet they typically have in common three characteristic components: cells, large amounts of amorphous ground substance, and protein fibers. The amount and structure of each component correlates with the function of the tissue, from the rigid ground substance in bones supporting the body to the inclusion of specialized cells; for example, a phagocytic cell that engulfs pathogens and also rids tissue of cellular debris.
Functions of Connective Tissues
Connective tissues perform many functions in the body, but most importantly, they support and connect other tissues; from the connective tissue sheath that surrounds muscle cells, to the tendons that attach muscles to bones, and to the skeleton that supports the positions of the body. Protection is another major function of connective tissue, in the form of fibrous capsules and bones that protect delicate organs and, of course, the skeletal system. Specialized cells in connective tissue defend the body from microorganisms that enter the body. Transport of fluid, nutrients, waste, and chemical messengers is ensured by specialized fluid connective tissues, such as blood and lymph. Adipose cells store surplus energy in the form of fat and contribute to the thermal insulation of the body.
Embryonic Connective Tissue
All connective tissues derive from the mesodermal layer of the embryo. The first connective tissue to develop in the embryo is mesenchyme , the stem cell line from which all connective tissues are later derived. Clusters of mesenchymal cells are scattered throughout adult tissue and supply the cells needed for replacement and repair after a connective tissue injury. A second type of embryonic connective tissue forms in the umbilical cord, called mucous connective tissue or Wharton’s jelly. This tissue is no longer present after birth, leaving only scattered mesenchymal cells throughout the body.
Classification of Connective Tissues
The three broad categories of connective tissue are classified according to the characteristics of their ground substance and the types of fibers found within the matrix (Table 1). Connective tissue proper includes loose connective tissue and dense connective tissue . Both tissues have a variety of cell types and protein fibers suspended in a viscous ground substance. Dense connective tissue is reinforced by bundles of fibers that provide tensile strength, elasticity, and protection. In loose connective tissue, the fibers are loosely organized, leaving large spaces in between. Supportive connective tissue —bone and cartilage—provide structure and strength to the body and protect soft tissues. A few distinct cell types and densely packed fibers in a matrix characterize these tissues. In bone, the matrix is rigid and described as calcified because of the deposited calcium salts. In fluid connective tissue , in other words, lymph and blood, various specialized cells circulate in a watery fluid containing salts, nutrients, and dissolved proteins.
Connective Tissue Proper
Fibroblasts are present in all connective tissue proper (Figure 1). Fibrocytes, adipocytes, and mesenchymal cells are fixed cells, which means they remain within the connective tissue. Other cells move in and out of the connective tissue in response to chemical signals. Macrophages, mast cells, lymphocytes, plasma cells, and phagocytic cells are found in connective tissue proper but are actually part of the immune system protecting the body.

Figure 1. Connective Tissue Proper. Fibroblasts produce this fibrous tissue. Connective tissue proper includes the fixed cells fibrocytes, adipocytes, and mesenchymal cells. LM × 400. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
The most abundant cell in connective tissue proper is the fibroblast . Polysaccharides and proteins secreted by fibroblasts combine with extra-cellular fluids to produce a viscous ground substance that, with embedded fibrous proteins, forms the extra-cellular matrix. As you might expect, a fibrocyte , a less active form of fibroblast, is the second most common cell type in connective tissue proper.
Adipocytes are cells that store lipids as droplets that fill most of the cytoplasm. There are two basic types of adipocytes: white and brown. The brown adipocytes store lipids as many droplets, and have high metabolic activity. In contrast, white fat adipocytes store lipids as a single large drop and are metabolically less active. Their effectiveness at storing large amounts of fat is witnessed in obese individuals. The number and type of adipocytes depends on the tissue and location, and vary among individuals in the population.
The mesenchymal cell is a multipotent adult stem cell. These cells can differentiate into any type of connective tissue cells needed for repair and healing of damaged tissue.
The macrophage cell is a large cell derived from a monocyte, a type of blood cell, which enters the connective tissue matrix from the blood vessels. The macrophage cells are an essential component of the immune system, which is the body’s defense against potential pathogens and degraded host cells. When stimulated, macrophages release cytokines, small proteins that act as chemical messengers. Cytokines recruit other cells of the immune system to infected sites and stimulate their activities. Roaming, or free, macrophages move rapidly by amoeboid movement, engulfing infectious agents and cellular debris. In contrast, fixed macrophages are permanent residents of their tissues.
The mast cell, found in connective tissue proper, has many cytoplasmic granules. These granules contain the chemical signals histamine and heparin. When irritated or damaged, mast cells release histamine, an inflammatory mediator, which causes vasodilation and increased blood flow at a site of injury or infection, along with itching, swelling, and redness you recognize as an allergic response. Like blood cells, mast cells are derived from hematopoietic stem cells and are part of the immune system.
Connective Tissue Fibers and Ground Substance
Three main types of fibers are secreted by fibroblasts: collagen fibers, elastic fibers, and reticular fibers. Collagen fiber is made from fibrous protein subunits linked together to form a long and straight fiber. Collagen fibers, while flexible, have great tensile strength, resist stretching, and give ligaments and tendons their characteristic resilience and strength. These fibers hold connective tissues together, even during the movement of the body.
Elastic fiber contains the protein elastin along with lesser amounts of other proteins and glycoproteins. The main property of elastin is that after being stretched or compressed, it will return to its original shape. Elastic fibers are prominent in elastic tissues found in skin and the elastic ligaments of the vertebral column.
Reticular fiber is also formed from the same protein subunits as collagen fibers; however, these fibers remain narrow and are arrayed in a branching network. They are found throughout the body, but are most abundant in the reticular tissue of soft organs, such as liver and spleen, where they anchor and provide structural support to the parenchyma (the functional cells, blood vessels, and nerves of the organ).
All of these fiber types are embedded in ground substance. Secreted by fibroblasts, ground substance is made of polysaccharides, specifically hyaluronic acid, and proteins. These combine to form a proteoglycan with a protein core and polysaccharide branches. The proteoglycan attracts and traps available moisture forming the clear, viscous, colorless matrix you now know as ground substance.
Loose Connective Tissue
Loose connective tissue is found between many organs where it acts both to absorb shock and bind tissues together. It allows water, salts, and various nutrients to diffuse through to adjacent or imbedded cells and tissues.
Adipose tissue consists mostly of fat storage cells, with little extracellular matrix (Figure 2). A large number of capillaries allow rapid storage and mobilization of lipid molecules. White adipose tissue is most abundant. It can appear yellow and owes its color to carotene and related pigments from plant food. White fat contributes mostly to lipid storage and can serve as insulation from cold temperatures and mechanical injuries. White adipose tissue can be found protecting the kidneys and cushioning the back of the eye. Brown adipose tissue is more common in infants, hence the term “baby fat.” In adults, there is a reduced amount of brown fat and it is found mainly in the neck and clavicular regions of the body. The many mitochondria in the cytoplasm of brown adipose tissue help explain its efficiency at metabolizing stored fat. Brown adipose tissue is thermogenic, meaning that as it breaks down fats, it releases metabolic heat, rather than producing adenosine triphosphate (ATP), a key molecule used in metabolism.
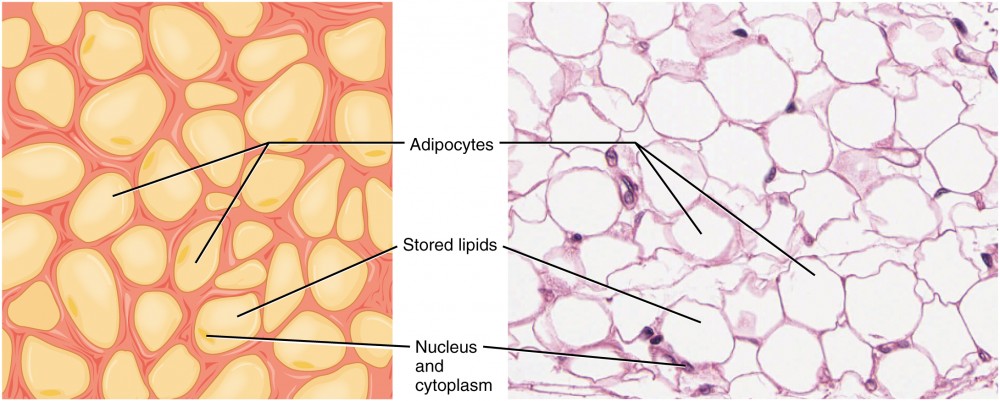
Figure 2. Adipose Tissue. This is a loose connective tissue that consists of fat cells with little extracellular matrix. It stores fat for energy and provides insulation. LM × 800. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Areolar tissue shows little specialization. It contains all the cell types and fibers previously described and is distributed in a random, web-like fashion. It fills the spaces between muscle fibers, surrounds blood and lymph vessels, and supports organs in the abdominal cavity. Areolar tissue underlies most epithelia and represents the connective tissue component of epithelial membranes, which are described further in a later section.
Reticular tissue is a mesh-like, supportive framework for soft organs such as lymphatic tissue, the spleen, and the liver (Figure 3). Reticular cells produce the reticular fibers that form the network onto which other cells attach. It derives its name from the Latin reticulus , which means “little net.”

Figure 3. Reticular Tissue. This is a loose connective tissue made up of a network of reticular fibers that provides a supportive framework for soft organs. LM × 1600. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Dense Connective Tissue
Dense connective tissue contains more collagen fibers than does loose connective tissue. As a consequence, it displays greater resistance to stretching. There are two major categories of dense connective tissue: regular and irregular. Dense regular connective tissue fibers are parallel to each other, enhancing tensile strength and resistance to stretching in the direction of the fiber orientations. Ligaments and tendons are made of dense regular connective tissue, but in ligaments not all fibers are parallel. Dense regular elastic tissue contains elastin fibers in addition to collagen fibers, which allows the ligament to return to its original length after stretching. The ligaments in the vocal folds and between the vertebrae in the vertebral column are elastic.
In dense irregular connective tissue, the direction of fibers is random. This arrangement gives the tissue greater strength in all directions and less strength in one particular direction. In some tissues, fibers crisscross and form a mesh. In other tissues, stretching in several directions is achieved by alternating layers where fibers run in the same orientation in each layer, and it is the layers themselves that are stacked at an angle. The dermis of the skin is an example of dense irregular connective tissue rich in collagen fibers. Dense irregular elastic tissues give arterial walls the strength and the ability to regain original shape after stretching (Figure 4).

Figure 4. Dense Connective Tissue. (a) Dense regular connective tissue consists of collagenous fibers packed into parallel bundles. (b) Dense irregular connective tissue consists of collagenous fibers interwoven into a mesh-like network. From top, LM × 1000, LM × 200. (Micrographs provided by the Regents of University of Michigan Medical School © 2012)
Disorders of the Connective Tissue: Tendinitis
Your opponent stands ready as you prepare to hit the serve, but you are confident that you will smash the ball past your opponent. As you toss the ball high in the air, a burning pain shoots across your wrist and you drop the tennis racket. That dull ache in the wrist that you ignored through the summer is now an unbearable pain. The game is over for now.
After examining your swollen wrist, the doctor in the emergency room announces that you have developed wrist tendinitis. She recommends icing the tender area, taking non-steroidal anti-inflammatory medication to ease the pain and to reduce swelling, and complete rest for a few weeks. She interrupts your protests that you cannot stop playing. She issues a stern warning about the risk of aggravating the condition and the possibility of surgery. She consoles you by mentioning that well known tennis players such as Venus and Serena Williams and Rafael Nadal have also suffered from tendinitis related injuries.
What is tendinitis and how did it happen? Tendinitis is the inflammation of a tendon, the thick band of fibrous connective tissue that attaches a muscle to a bone. The condition causes pain and tenderness in the area around a joint. On rare occasions, a sudden serious injury will cause tendinitis. Most often, the condition results from repetitive motions over time that strain the tendons needed to perform the tasks.
Persons whose jobs and hobbies involve performing the same movements over and over again are often at the greatest risk of tendinitis. You hear of tennis and golfer’s elbow, jumper’s knee, and swimmer’s shoulder. In all cases, overuse of the joint causes a microtrauma that initiates the inflammatory response. Tendinitis is routinely diagnosed through a clinical examination. In case of severe pain, X-rays can be examined to rule out the possibility of a bone injury. Severe cases of tendinitis can even tear loose a tendon. Surgical repair of a tendon is painful. Connective tissue in the tendon does not have abundant blood supply and heals slowly.
While older adults are at risk for tendinitis because the elasticity of tendon tissue decreases with age, active people of all ages can develop tendinitis. Young athletes, dancers, and computer operators; anyone who performs the same movements constantly is at risk for tendinitis. Although repetitive motions are unavoidable in many activities and may lead to tendinitis, precautions can be taken that can lessen the probability of developing tendinitis. For active individuals, stretches before exercising and cross training or changing exercises are recommended. For the passionate athlete, it may be time to take some lessons to improve technique. All of the preventive measures aim to increase the strength of the tendon and decrease the stress put on it. With proper rest and managed care, you will be back on the court to hit that slice-spin serve over the net.
Watch this animation to learn more about tendonitis, a painful condition caused by swollen or injured tendons.
https://youtu.be/p5vnf0VLvxQ
Supportive Connective Tissues
Two major forms of supportive connective tissue, cartilage and bone, allow the body to maintain its posture and protect internal organs.
The distinctive appearance of cartilage is due to polysaccharides called chondroitin sulfates, which bind with ground substance proteins to form proteoglycans. Embedded within the cartilage matrix are chondrocytes , or cartilage cells, and the space they occupy are called lacunae (singular = lacuna). A layer of dense irregular connective tissue, the perichondrium, encapsulates the cartilage. Cartilaginous tissue is avascular, thus all nutrients need to diffuse through the matrix to reach the chondrocytes. This is a factor contributing to the very slow healing of cartilaginous tissues.
The three main types of cartilage tissue are hyaline cartilage, fibrocartilage, and elastic cartilage (Figure 5). Hyaline cartilage , the most common type of cartilage in the body, consists of short and dispersed collagen fibers and contains large amounts of proteoglycans. Under the microscope, tissue samples appear clear. The surface of hyaline cartilage is smooth. Both strong and flexible, it is found in the rib cage and nose and covers bones where they meet to form moveable joints. It makes up a template of the embryonic skeleton before bone formation. A plate of hyaline cartilage at the ends of bone allows continued growth until adulthood. Fibrocartilage is tough because it has thick bundles of collagen fibers dispersed through its matrix. The knee and jaw joints and the the intervertebral discs are examples of fibrocartilage. Elastic cartilage contains elastic fibers as well as collagen and proteoglycans. This tissue gives rigid support as well as elasticity. Tug gently at your ear lobes, and notice that the lobes return to their initial shape. The external ear contains elastic cartilage.

Figure 5. Types of Cartilage. Cartilage is a connective tissue consisting of collagenous fibers embedded in a firm matrix of chondroitin sulfates. (a) Hyaline cartilage provides support with some flexibility. The example is from dog tissue. (b) Fibrocartilage provides some compressibility and can absorb pressure. (c) Elastic cartilage provides firm but elastic support. From top, LM × 300, LM × 1200, LM × 1016. (Micrographs provided by the Regents of University of Michigan Medical School © 2012)
Bone is the hardest connective tissue. It provides protection to internal organs and supports the body. Bone’s rigid extracellular matrix contains mostly collagen fibers embedded in a mineralized ground substance containing hydroxyapatite, a form of calcium phosphate. Both components of the matrix, organic and inorganic, contribute to the unusual properties of bone. Without collagen, bones would be brittle and shatter easily. Without mineral crystals, bones would flex and provide little support. Osteocytes, bone cells like chondrocytes, are located within lacunae. The histology of transverse tissue from long bone shows a typical arrangement of osteocytes in concentric circles around a central canal. Bone is a highly vascularized tissue. Unlike cartilage, bone tissue can recover from injuries in a relatively short time.
Cancellous bone looks like a sponge under the microscope and contains empty spaces between trabeculae, or arches of bone proper. It is lighter than compact bone and found in the interior of some bones and at the end of long bones. Compact bone is solid and has greater structural strength.
Fluid Connective Tissue

Figure 6. Blood: A Fluid Connective Tissue. Blood is a fluid connective tissue containing erythrocytes and various types of leukocytes that circulate in a liquid extracellular matrix. LM × 1600. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
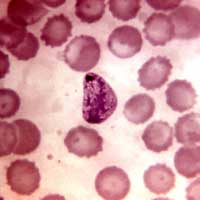
Blood and lymph are fluid connective tissues. Cells circulate in a liquid extracellular matrix. The formed elements circulating in blood are all derived from hematopoietic stem cells located in bone marrow (Figure 6). Erythrocytes, red blood cells, transport oxygen and some carbon dioxide. Leukocytes, white blood cells, are responsible for defending against potentially harmful microorganisms or molecules. Platelets are cell fragments involved in blood clotting. Some white blood cells have the ability to cross the endothelial layer that lines blood vessels and enter adjacent tissues. Nutrients, salts, and wastes are dissolved in the liquid matrix and transported through the body.
Lymph contains a liquid matrix and white blood cells. Lymphatic capillaries are extremely permeable, allowing larger molecules and excess fluid from interstitial spaces to enter the lymphatic vessels. Lymph drains into blood vessels, delivering molecules to the blood that could not otherwise directly enter the bloodstream. In this way, specialized lymphatic capillaries transport absorbed fats away from the intestine and deliver these molecules to the blood.
Self-Check Questions
Take the quiz below to check your understanding of Connective Tissue:
- Anatomy & Physiology. Authored by : OpenStax College. Provided by : Rice University. Located at : http://cnx.org/contents/[email protected] . License : CC BY: Attribution . License Terms : Download for free at http://cnx.org/contents/[email protected]
- To save this word, you'll need to log in. Log In
wandering cell
Medical Definition of wandering cell
Dictionary entries near wandering cell.
wandering pacemaker
Cite this Entry
“Wandering cell.” Merriam-Webster.com Medical Dictionary , Merriam-Webster, https://www.merriam-webster.com/medical/wandering%20cell. Accessed 9 Apr. 2024.
Subscribe to America's largest dictionary and get thousands more definitions and advanced search—ad free!

Can you solve 4 words at once?
Word of the day.
See Definitions and Examples »
Get Word of the Day daily email!
Popular in Grammar & Usage
The tangled history of 'it's' and 'its', more commonly misspelled words, why does english have so many silent letters, your vs. you're: how to use them correctly, every letter is silent, sometimes: a-z list of examples, popular in wordplay, the words of the week - apr. 5, 12 bird names that sound like compliments, 10 scrabble words without any vowels, 12 more bird names that sound like insults (and sometimes are), 8 uncommon words related to love, games & quizzes.


An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.34(4); 1921 Sep 30

WANDERING CELLS, ENDOTHELIAL CELLS, AND FIBROBLASTS IN CULTURES FROM HUMAN LYMPH NODES
Wandering cells migrate from cultures of human lymph nodes after 2 or 3 hours incubation; they are actively ameboid and phagocytic. Endothelial cells appear in the plasma clot after 24 to 48 hours incubation. They are relatively inactive and less phagocytic. Fibroblasts are seen after 48 hours incubation. They are inactive and not phagocytic. The probable origin of wandering cells from endothelial cells is discussed.
The Full Text of this article is available as a PDF (886K).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Lewis WH, Webster LT. GIANT CELLS IN CULTURES FROM HUMAN LYMPH NODES. J Exp Med. 1921 Feb 28; 33 (3):349–360. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Wandering cell
In anatomy and histology , the term wandering cell (or ameboid cell ) is used to describe cells that are found in connective tissue , but are not fixed in place. This term is used occasionally and usually refers to blood leukocytes (which are not fixed and organized in solid tissue) in particular mononuclear phagocytes. Frequently, the term refers to circulating macrophages and has been used also for stationary macrophages fixed in tissues ( histiocytes ), which are sometimes referred to as "resting wandering cells".
- Connective tissue cells
Connective tissue cells are typically divided into two types, fixed cells and wandering cells. Fibrocytes, or fibroblasts and fat cells(adipocytes) are fixed cells, where as macrophages, monocytes, lymphocytes, plasma cells, eosinophils and mast cells are wandering cells. Fibrocytes are the most common cell type in connective tissues. If fibrocytes are stimulated by damage to the surrounding tissue, the fibrocyte is altered into a fibroblast. The fibroblasts contain organelles that are necessary for the synthesis and excretion of proteins needed to repair the tissue damage. Fibrocytes usually do not leave the connective tissue. Reticular cells are usually larger than fibrocytes. Reticular cells are the fibrocytes of reticular connective tissue and form a network of reticular fibers. Adipocytes are fat cells that are fixed cells in loose connective tissue. Their main function is the storage of lipid. Macrophages arise from monocytes. Monocytes originate in the bone marrow upon which they are released into the blood stream. They are mobile and leave the blood stream to enter connective tissues where they differentiate into macrophages. The fibroblasts are the most important in the connective tissue. Fibroblasts manufacture and maintain the extracellular material. They migrate throughout the extracellular matrix to wherever they are needed. Adipocytes are cells that are very efficient at storing energy in the form of triglycerides.
Types of cells
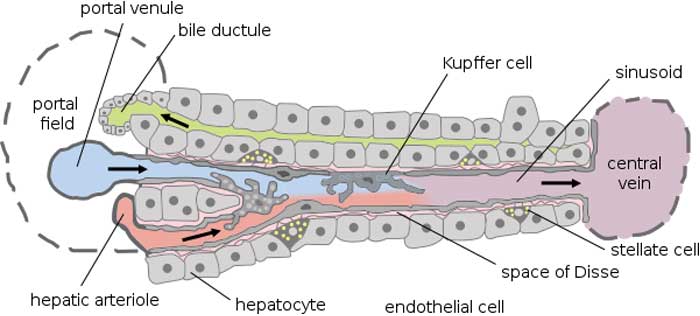
Macrophages: Supported by a network of connective tissue. Understood as the Reticuloendothelial System, the RES allows microglial differential in the CNS, pulmonary alveolar macrophages, tissue histiocytes, Kupffler Hepatic macrophages, Glomerular Mesangial Proliferation and unnamed Splenic expression of wandering macrophages. Sharing of iron storage remains an essential mystery.
Lymphocytes: These are cells responsible for immune responses that circulate in the blood. Normally, only small numbers are found in the CTs throughout the body. The number increases dramatically at certain sites of tissue inflammation. They are also very numerous in the lamina propria of the respiratory and gastrointestinal tracts, where they are involved in immunosurveillance. The lamina propria is a layer of loose CT lying immediately beneath the epithelium.
Plasma cells: Plasma cells are derived from B-lymphocytes and produce antibodies against a specific antigen. They have a limited migratory ability and a short life.
Neutrophils: Neutrophils are white blood cells that act as phagocytes in the early stages of acute inflammation.
Eosinophils: Eosinophils are white blood cells that are found in the lamina propria of the GI tract, and at sites of allergic reaction and parasitic infection.
Basophils: Basophils are white blood cells that are similar to mast cells in having vasoactive agents released in response to an allergen.
Monocytes: Monocytes are white blood cells that will give rise to all the phagocytes of the mononuclear phagocytic system (see Ross et al., pg. 110, and Table 5.4, pg. 112). In CT, they give rise to macrophages (histiocytes).
Characteristics
Wandering Cells are probably amoeboid when alive but after fixations they are seen to possess a distinct nucleus. These cells are regarded as a special type of blood cell. The cells were found to take up iron saccharate, which had been injected into the hemocoele. The cell's cytoplasm contains a variety of inclusions and characteristically, a well-marked eosinophile area. The wandering cells of nudibranchs are excretory taking up effete matter from the hemocoele and discharging it into the lumen of the gut.
Lymphocytes
Lymphocytes are just one group of cells that function as part of the immune system. More of this group travel around the lymphatic system than in the blood network. Two types of lymphocytes are present in the bloodstream, which are the B cells and the T cells.
B cells are wandering cells that are antibody factories. They are capable of producing molecules that can recognize and bond to specific types of molecules present in infectious organisms or substances that the body identifies as foreign. Every individual B cell makes only one particular type of antibody, specific to only one type of foreign substance. For example, where one cell produces antibody against one of the many viral causes of a cold, another cell's antibodies will ignore the presence of the same virus completely. Normally, the body contains many different B cells, specialized for a specific invader, but only has low levels of each type circulating. When an invader manages to break past other defenses, like the skin or digestive tract into the body, then the circulating B cells that target that particular foreigner multiply up and produce more antibody. Special forms of B cell called plasma cells produce antibodies; little versions of the specialized B cells, called memory B cells, remain stored in lymph glands prepared for the next invasion by the foreigner. Although the products of B cells, the antibodies, stick onto their target invader, they most often do not kill the invader. This job falls to other types of lymphocytes called T cells. There are three different forms of T cells, which are the Helper T cells, the Killer T cells, and the Suppressor T cells. [ citation needed ]
- Mesenchymal
This page was last updated at 2024-04-06 10:42 UTC. Update now . View original page .
All our content comes from Wikipedia and under the Creative Commons Attribution-ShareAlike License .
If mathematical, chemical, physical and other formulas are not displayed correctly on this page, please use Firefox or Safari
- Branches of Biology
- Importance of Biology
- Domain Archaea
- Domain Eukarya
- Biological Organization
- Biological Species Concept
- Biological Weathering
- Cellular Organization
- Cellular Respiration
- Types of Plants
- Plant Cells Vs. Animal Cells
- Prokaryotic Cells Vs. Eukaryotic Cells
- Amphibians Vs. Reptiles
- Anatomy Vs. Physiology
- Diffusion vs. Osmosis
- Mitosis Vs. Meiosis
- Chromosome Vs. Chromatid
- History of Biology
- Biology News

- Cell Biology
Kupffer Cells In Liver: Definition, Development, Anatomy, and Functions
Kupffer Cells : Every day, living organisms like humans are subject to the attack of disease-causing agents called pathogens . The only good thing is that they have a special kind of innate protection referred to as “ immunity .”
As the organisms’ complexity level increases, their immunity also becomes more extensive. Humans, for example, have various cells in the body which act to help deter the presence of pathogens.
Coming from the two Greek words “ makro ” and “ phagein ” which mean “ big ” and “ to eat ” respectively, macrophages are large and specialized cells for destroying and engulfing foreign bodies. Check out the complete history of immunology and its timeline here.
They are usually formed as a response to an infection or an accumulation of dead and damaged cells. Interestingly, macrophages in the body are modified to different structures and forms to adapt to various microorganisms and invaders.
For instance, macrophages in the liver sinusoids are called Kupffer cells .
How to pronounce Kupffer Cells?
What are Kupffer Cells?
In mammalian bodies, Kupffer cells are the most abundant tissue macrophages as they constitute 80-90% of them. Also known as Kupffer-Browicz cells or stellate macrophages , these specialized macrophages are specifically found in the liver.
As identified in the early 1970s, the specialized function of Kupffer cells is mainly due to their peroxidase activity. In biology, this is termed the “tolerogenic” phentotype necessary to prevent undesired immune response to any stimuli.
They are identified to contain vacuoles and granules and tubular and vermiform (worm-like) invaginations.
Discovery of Kupffer Cells
Twenty-two years later, such an idea was disproved by scientist Tadeusz Browicsz as he correctly identified them as macrophages.
Development of Kupffer Cells
In humans and other mammals, the development of Kupffer cells starts in the yolk sac. Primitive macrophages differentiate into fetal macrophages and then enter the bloodstream. After that, they go to the fetal liver to become mature cells.
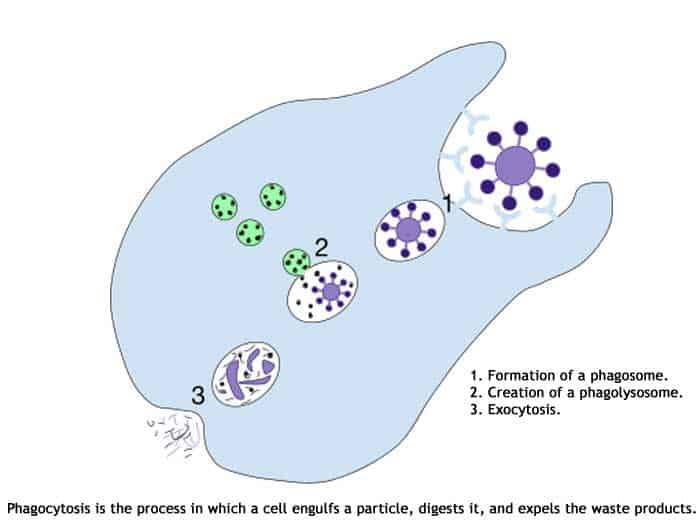
Here is an overview of Phagocytosis:
Anatomy of Kupffer Cell
These cells are too minute to be observed individually using a compound microscope. Often, electron microscopy is to observe the Kupffer cells elongated to worm-like to the star-shaped body.
Like any other cells, they have various distributions and arrangements of organelles. Described below are some of them.

Plasma Membrane
They have plasma membranes with extensions like microvilli , pseudopodia , filopodia , and lamellipodia . These structures are what give them a star-like to worm-like appearance.
They are the largest sinusoidal cells, hence, their cytoplasmic volume is generally dense and considerable. Aside from that, their cytoplasm contains a large number of lysosomes (for degradation of organelles and removal of wastes), vacuoles (storage of materials and wastes ), and phagosomes (involved in the engulfment of foreign bodies).

Golgi Bodies
In Kupffer cells, the Golgi bodies are seen observed to be in groups near the nucleus. In the cell, the Golgi bodies are involved in the secretion and intracellular transport of vesicles .

Rough Endoplasmic Reticulum (RER)
Known to be the organelle responsible for ribosome (for protein synthesis) synthesis, the rough ER is very abundant in Kupffer cells.

Like most animal cells, they contain only a single nucleus. Their nuclei are mostly oval-shaped and have finely distributed euchromatin . It is the nucleus that contains the genetic information which is responsible for the expression of traits.

Other Organelles
Other organelles like the free ribosomes (for protein synthesis), mitochondria (for ATP/ energy production), and microtubules (for the transport of other organelles) are dispersed in the cytoplasm . Check out the cellular respiration equation here. Kupffer cells do not contain glycogen and fat droplets, unlike other liver cells.
Functions of Kupffer Cells
Aside from digestion , detoxification, and storage, the liver can function for immunity through the Kupffer cells. The following are ways in which such cells contribute to immune function.
1. To remove protein complexes and small particles from blood
- This function is important because the blood that passes through that vein is rich with pathogen-derived products like lipopolysaccharides and proteins.
- Such products must be removed from circulation to prevent systemic immune activation.
2. To capture and digest microorganisms and worn-out cells
- In addition, because of their peroxidase activity in the cytoplasm, they can degrade bacterial and other microorganism walls.
3. To modulate iron homeostasis in the liver
- Hepcidin is a peptide hormone that primarily controls the entry of iron in the circulatory system of mammals. Interestingly, when hepcidin levels increase (especially during inflammation or immune response), serum iron and the absorption of iron in the gut decreases.
- However, at present, that suppressing molecule produced by Kupffer cells is not yet identified.
4. To regulate anti-viral immunity during Hepatitis B and C infections
- Together with other macrophages, they contribute to the tissue damage of the infected body part. Aside from that, they also regulate fibrosis (thickening of connective tissue), cirrhosis (scarring of the liver), and hepatocellular carcinoma (abnormal growth of liver cells), which all happen during hepatitis.
- However, the exact mechanisms of how Kupffer cells mediate these infections remain unclear and are still up for further studies.
As mentioned above, Kupffer cells exhibit great adaptability depending primarily on their immune environment. But despite medical practices and technology advancements, understanding the exact mechanisms of their functions is still very rudimentary.
Hence, future studies should promote novel insights into the potential of Kupffer cells for therapeutic manipulation. Wouldn’t that be great?
Cite This Page
- [1] – Robertson, Sally. “ What Is a Macrophage? ” News-Medical.net. 2014. Accessed December 13, 2016. Link .
- [2] – “ Role of Kupffer Cells in Host Defense and Liver Disease. ” Liver International: Official Journal of the International Association for the Study of the Liver. Accessed December 13, 2016. Link .
- [3] – Dixon, Laura J., Mark Barnes, Hui Tang, Michele T. Pritchard, and Laura E. Nagy. “ Kupffer Cells in the Liver. ” Comprehensive Physiology. 2013. Accessed December 13, 2016. Link .
- [4] – The Discovery of Kupffer Cells – “ Hepatocyte and Kupffer Cell Interactions ” – Link .
- [5] – “ Development, Differentiation, and Maturation of Kupffer Cells. ” Microscopy Research and Technique. Accessed December 13, 2016. Link .
- [6] – “ The role of Kupffer cells in hepatitis B and hepatitis C virus infections ” – PDF .
- [7] – “ Liver. ” InnerBody. Accessed December 13, 2016. Link .
- [8] – “ Kupffer cells modulate iron homeostasis in mice via regulation of hepcidin expression “- Link .
RELATED ARTICLES MORE FROM AUTHOR

Top Cell Biology News of 2020 – A Round Up
Top 10 Cell Biology Discoveries in 2019

Explore The Top 8 Functions of Golgi Apparatus
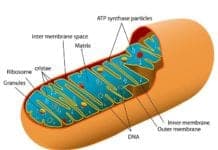
Explore Mitochondria Functions & Their Importance

Top 15 Discoveries in Cell Biology for 2018
Types of Bone Cells
Leave a reply cancel reply.
Save my name, email, and website in this browser for the next time I comment.
By using this form you agree with the storage and handling of your data by this website. *
Recent Posts

Blooming Texas: 25 Gorgeous Native Flowers Revealed!

Exploring the Top 50 Most Exquisite Purple Flowers in the World

Top 21 Holly Flowers For Sprucing Up Your Garden!

The Enchanting Beauty of the Top White Flowers
What Is Biological Magnification?

Top 34 Flightless Birds of All Times!

25 Reasons That Emphasizes The Importance of Biology

Top 27 Biology-themed Movies

Biology Boomtowns: 10 Best US Cities for Job Opportunities
Uncovering the Fathers of Biology: The Geniuses Who Unveiled Life’s Secrets
25 Mind-Blowing Biology Breakthroughs That Shaped Our World!

The Ultimate Guide: Discover 162+ Doctor Specialties for Every Health Need
40 Different Types of Birds
334 Types of Monkeys
Biology history.

History of Anatomy
History of Biochemistry

History of Biotechnology
History of Botany

History of Cell Biology

History of Ecology
Complete History of Evolution

History of Genetics
History of Immunology

History of Microbiology
- Privacy Policy
Anatomy 214-Final Exam 1

IMAGES
VIDEO
COMMENTS
Wandering cell. In anatomy and histology, the term wandering cell (or ameboid cell) [1] is used to describe cells that are found in connective tissue, but are not fixed in place. This term is used occasionally and usually refers to blood leukocytes (which are not fixed and organized in solid tissue) in particular mononuclear phagocytes.
Definition. Connective tissue is found between other tissue types and organs. It contains high quantities of water, several types of cells, and a fibrous extracellular matrix. The connective tissue of an organ is usually referred to as the stroma. This tissue type can have very different structures according to the proportions of its components.
The cells of connective tissues are of two types; fixed or stationary or resident cells and transient or motile or wandering cells. A. Fixed cells (or resident cells) Fixed or resident connective tissue cells are the cells that originate from local mesenchyme and are permanent residents of connective tissues.
Photomicrograph of a Healing Fracture A healing fracture requires the use of a range of connective tissue subtypes to help to stabilise and restore function to the damaged bone. This includes dense irregular connective tissue, cartilaginous tissue and bone tissue. Note the bright red tissue in the centre of the image - this is cartilaginous tissue forming a bridge across the fracture gap.
Protection is another major function of connective tissue, in the form of fibrous capsules and bones that protect delicate organs and, of course, the skeletal system. Specialized cells in connective tissue defend the body from microorganisms that enter the body. Transport of fluid, nutrients, waste, and chemical messengers is ensured by ...
Wandering cells move throughout the connective tissue matrix. Macrophages, which eat dead and harmful cells, as well as the cells which make up blood connective tissue are examples of wandering cells.
Examination of Cornea: The limbal region should be examined in cases of suspected vitamin B 2 deficiency where vessels grow straight out from the limbal arches all around the cornea of each eye. Corneal corpuscles can be seen and wandering cells that have entered in response to inflammation. The corneal nerves are visible dividing dichotomously, and blood vessels otherwise invisible can be ...
Post the Definition of wandering cell to Facebook Facebook. Share the Definition of wandering cell on Twitter Twitter. Love words? Need even more definitions? Subscribe to America's largest dictionary and get thousands more definitions and advanced search—ad free! Merriam-Webster unabridged.
This cell layer is essential for absorption, excretion, and gaseous exchange; it is therefore vital to maintain defensive cells just below the vulnerable surface. Fat cells may occur singly or in small or large numbers. When fat cells predominate, the tissue is called adipose tissue. One of the special connective tissues, adipose tissue, serves ...
Connective tissue - Migrating Cells, Fibers, Matrix: In addition to the relatively fixed cell types described above, there are free cells that reside in the interstices of loose connective tissue. These vary in their abundance and are free to migrate through the extracellular spaces. Among these wandering cells are the mast cells; these have a cell body filled with coarse granules that contain ...
wandering cell: a cell such as a leukocyte, having ameboid movements, with a power of locomotion. Synonym(s): wandering cell Synonym(s): migratory cell
Mononuclear wandering cells soon migrate into the mesenchyme. Crypts proliferate into the connective tissue and are infiltrated by T-lymphocytes at week 16. The developing palatine tonsils are considered the first B-cell regions in fetal lymphoid tissue. This series of developmental steps for the palatine tonsils arises from the 2nd pharyngeal ...
Anatomy of a neuron. Neurons (or nerve cells) are specialized cells that transmit and receive electrical signals in the body. Neurons are composed of three main parts: dendrites, a cell body, and an axon. Signals are received through the dendrites, travel to the cell body, and continue down the axon until they reach the synapse (the ...
8 terms · fibroblasts → produce fibers, fixed macrophages → phagocytize pathogens and dama…, adipocytes → fat cells, mesenchymal cells → stem cells that respond to inj…, free macrophages → roam tissues and gather at sit…
cell, in biology, the basic membrane-bound unit that contains the fundamental molecules of life and of which all living things are composed.A single cell is often a complete organism in itself, such as a bacterium or yeast.Other cells acquire specialized functions as they mature. These cells cooperate with other specialized cells and become the building blocks of large multicellular organisms ...
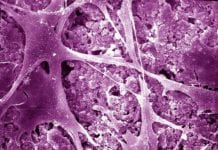
A metastasis occurs when cells from the primary tumor escape into the bloodstream and take up residence in a different part of the body, growing into a secondary or metastatic tumor. The reason that metastases are so worrisome is that these secondary tumors are often more aggressive, faster-growing, and more difficult to treat. And more deadly.
Abstract. Wandering cells migrate from cultures of human lymph nodes after 2 or 3 hours incubation; they are actively ameboid and phagocytic. Endothelial cells appear in the plasma clot after 24 to 48 hours incubation. They are relatively inactive and less phagocytic. Fibroblasts are seen after 48 hours incubation.
Ependymal cells are mostly known as a specialized type of epithelial tissue.They are indispensable components of the central nervous system (CNS) and originate from neuroepithelial cells of the neural plate.. Ependymal cells are found lining the central canal of the spinal cord and ventricles of the brain. The choroid plexus is formed by vascularized invaginations of this neuroepithelium and ...
Ependymal Cell. An ependymal cell is a type of glial cell that forms the ependyma, a thin membrane that lines the ventricles of the brain and the central column of the spinal cord. Their main function is to secrete, circulate, and maintain homeostasis of the cerebrospinal fluid that fills the ventricles of the central nervous system.
Splenic macrophages - located in the red and white pulp of the spleen. The main function of macrophages reflects in the process of phagocytosis which protects the tissues from infection and injury by ingesting and destroying the pathogens (e.g., bacteria), dying or dead cells or cellular debris. In addition, the macrophages also play a key role ...
In anatomy and histology, the term wandering cell (or ameboid cell) is used to describe cells that are found in connective tissue, but are not fixed in place.This term is used occasionally and usually refers to blood leukocytes (which are not fixed and organized in solid tissue) in particular mononuclear phagocytes.
2. To capture and digest microorganisms and worn-out cells. As macrophages, Kupffer cells can engulf and break down old red blood cells that pass through the liver sinusoids. In addition, because of their peroxidase activity in the cytoplasm, they can degrade bacterial and other microorganism walls. 3.
Body cavities __. A. are internal chambers containing many vital organs. B. includes a ventral space and its subdivisions. C. allow visceral organs to change size and shape. D. all of the above. D. all of the above. The major function of the ___ system is the internal transport of nutrients, wastes, and gases.