- Skip to main content
- Skip to header right navigation
- Skip to after header navigation
- Skip to site footer

Ask the Dentist
Health Begins in the Mouth | Dr. Mark Burhenne
Every product I recommend meets my rigorous safety and testing standards. When you buy through links on my website, I may earn a small commission which helps offset the costs of running this website. Learn more →

Pain After Dental Work: Types, Recovery Time, & Pain Relief
Get Dr. B’s Dental Health Tips
1. jaw muscle fatigue, 2. pulpitis, 3. referred myofacial pain, 4. dry socket pain, 5. soft tissue injury pain, 6. dental implant pain, 7. gum graft surgery pain, 9. tooth sensitivity, how to prevent pain after a dental visit, how to relieve pain after dental work.
The number one reason people put off going to the dentist is a fear of pain . This can greatly damage your oral health and lead to many more problems down the road.
Some pain after a dental visit is to be expected, while other types of pain after dental work may require follow-up care.
You may wonder if your jaw pain or referred pain in your ears, eyes, or other areas of the face is normal, rare, or cause for alarm.
The most common types of pain after a dental visit include:
Common causes of pain after dental work are poor procedure, pre-existing inflammation, very large cavities, and irritation of TMD (TMJ pain).
People who struggle with teeth grinding/clenching are generally at the highest risk for postoperative pain.
IF YOU PURCHASE A PRODUCT USING A LINK BELOW, WE MAY RECEIVE A SMALL COMMISSION AT NO ADDITIONAL COST TO YOU. READ OUR AD POLICY HERE .
How long does pain after dental work last.
The majority of pain after dental treatment should go away in 1-2 days. For wisdom tooth surgery, pain may last closer to 1-2 weeks. If you have TMJ pain after dental work, it may take months for the pain to go away.
Typically, I recommend asking the dentist who will perform your procedure what kind of pain you should expect afterwards.
In addition, understanding what kind of pain to expect helps you know when your dental problems are cause for a follow-up visit.
Questions to ask your dentist include:
- Will I feel stabbing pain?
- Should I expect a sore mouth?
- Will my teeth be sensitive to hot or cold?
- Should my recovery pain make it hard to perform daily tasks, or is it more likely to simply be annoying or minor?
If you experience pain outside of what your dentist describes as expected, call him or her to find out the next steps. If procedures have been performed poorly or if you have additional issues that must be corrected professionally, you may end up having to get a follow-up procedure.
Free weekly dental health advice in your inbox, plus 10 Insider Secrets to Dental Care as a free download when you sign up

What it is: Jaw muscle pain after dental work, like a filling or root canal, is muscle soreness caused by having the mouth open for a long time. People that grind their teeth a lot are more susceptible to this condition because their temporomandibular joint is already strained.
What it feels like: The jaw muscles give out, much like your leg muscles when running until you can hardly stand. Your muscles may feel tired, exhausted, and shaking, which produces pain.
How it happens: The mouth stays open for an extended period of time, exhausting the muscles of the jaw.
Your dentist may notice when this is happening during a procedure because you won’t be able to keep your mouth open and have accompanying muscle spasms. You may believe you’re holding your mouth open, even when you aren’t.
How to fix it: If you know you have TMJ problems, ask your dentist for a bite block. A bite block is a small rubber block that does not force your jaw open but allows it to stay open without jaw muscle exhaustion. The block does the work for you.
How long should jaw muscle fatigue last? Jaw muscle pain after dental work is most common for longer procedures, like root canals, and can last for several days.
What it is: Pulpitis is inflammation of the sensitive inner layer, or pulp, of the tooth.
What it feels like: Pulpitis causes sensitive teeth , painful when exposed to hot or cold. It can also cause generalized toothache and may eventually lead to an abscess if left untreated. This painful condition will usually be concentrated to the tooth your dentist worked on during the procedure.
The pain of pulpitis after dental work is similar to the pain you develop from extensive tooth decay.
There are two types of pulpitis: reversible pulpitis and irreversible pulpitis. If you have reversible pulpitis, you probably don’t feel pain unless something actually touches your affected tooth. Irreversible pulpitis feels more consistent and hurts worse.
How it happens: Even a simple filling can cause pulpitis. Aggressively prepping and drilling of the tooth can cause pulpitis. Your dentist also may have used a lot of air after drilling in the tooth, which can cause tooth pain to be generated from the filled area of the tooth.
Rarely, a careless dentist may actually nick the nerve, leading to greater sensitivity and pain.
However, your dentist may find that a cavity is deeper and more extensive than originally thought, requiring the tooth be drilled into the nerve area. This would require a root canal.
Working on a cracked or chipped tooth may also cause pulpitis.
How to fix it: Reversible pulpitis can go away if the inflammation goes down, but your dentist will probably need to examine and correct the damage if possible. Irreversible pulpitis, once the inflammation reaches a certain point, requires a root canal or tooth extraction .
How long should pulpitis last? Pulpitis pain in a specific tooth several days after a dental procedure necessitates another visit to the dentist. Neither type of pulpitis is likely to go away on its own.
What it is : Any dental procedure may result in referred facial pain. This is pain that may affect the eye socket, ears, or other facial areas.
What it feels like: Referred myofacial pain may feel like an earache or other persistent pain in areas associated with the teeth, but outside of the mouth.
How it happens: This happens when nerves are inflamed or irritated by dental work but send pain throughout other nerves nearby. It can feel like a knotted muscle and will probably interfere with your sleep.
There’s no way to predict or prevent referred pain after a dental visit.
How to fix it : While this type of pain is very common, it’s also one that will require intervention from your dentist or oral surgeon.
Common ways to treat referred myofascial pain include trigger point injections and physical therapy.
How long should referred myofacial pain last? Referred myofacial pain after dental work probably won’t go away without further treatment.
What it is: Dry socket is bone pain that results from loss of the blood clot in a tooth socket after tooth extraction. This pain after dental visits is usually associated with more extensive oral surgery (like after wisdom teeth removal ).
What it feels like: Dry socket pain is deep, sore pain that radiates from your tooth socket up and down the same side of your face.
The pain receptors in bone are very sensitive, which is why this condition hurts so much.
Dry socket pain sometimes radiates up to the ear and may also cause worsened breath or unpleasant taste in the mouth. Other symptoms include headache and, on occasion, fever from a resulting infection.
How it happens: If the blood clot from your tooth extraction falls out before the 4-day mark after tooth extraction, you will probably develop dry socket. It’s most likely 2-3 days after your tooth is removed.
Any sucking motion in the mouth, like drinking through a straw or aggressive mouthwash swishing increases your chances of losing the blood clot over your exposed bone.
How to fix it: Dry socket that happens in the first 1-2 days after extraction will probably need to be corrected by your dentist or oral surgeon. Most of the time, he or she can use dry socket paste to relieve your pain and protect the exposed area so it has time to heal.
In severe cases, you may need bone graft material or surgical foam to support the healing process. This is most necessary for people with thinning bone (like those with advanced periodontal disease).
If your clot falls out between day 3-4, the pain is likely to clear up on its own without intervention. However, it’s always a good idea to contact your dentist/oral surgeon to find out what s/he would suggest.
Home remedies for dry socket pain may include over-the-counter anti-inflammatory medications, cold compress, salt water rinse, clove oil, and/or honey.
How long should dry socket pain last? Dry socket is typically painful for 7-10 days after tooth extraction. Patients with advancing gum disease may experience pain for several weeks.
What it is: Nicking the gums or tongue during a dental procedure will likely cause trauma in the mouth, resulting in soft tissue pain.
What it feels like: Injury of soft tissue typically results in throbbing pain that’s sensitive to touch, like when you chew food. It will probably also cause pain when you eat hot foods.
Anytime the tongue is harmed at all can be very painful. It’s one of the reasons your dentist discourages eating food that requires a lot of chewing following a procedure that requires anesthetic.
How it happens: Some people may inadvertently bite their tongues during a dental procedure, which will produce pain in the days following the procedure as the tongue heals. The gums may be nicked by dental instruments.
Gums will also feel pain after procedures where they are purposefully incised, such as removal of an impacted wisdom tooth.
Burning your mouth with hot foods shortly after a procedure can also cause pain.
A biopsy usually does not cause a lot of pain, but there is the possibility of soft tissue involvement, which can cause pain as it heals.
How to fix it: Be very cautious eating after dental work where your mouth and tongue are numbed. Use a salt water rinse, clove oil, benzocaine, or another toothache home remedy to correct the pain.
How long should soft tissue injury pain last? Soft tissue pain should last 3 days or fewer, although it can open your body up to infection. The tongue is very sensitive and takes a while to heal, which can take 2-3 weeks.
If you develop an infection from this type of injury, your dentist will probably prescribe an antibiotic.
Numbness in the tongue, lips, and jaw (known as paresthesia) is normal for a few hours after many types of dental procedures. However, if it lasts much longer, it may be permanent. If this happens, talk to your dentist right away.
What it is: When you get a dental implant , you’ll have soreness in the days following the procedure.
What it feels like: Implant pain is inflammation in the bone, like dry socket, and bone pain is very generalized. It can refer, run up and down the jaw, and is very achy, which is the nature of bone pain.
The pain receptors in bone are one of the most sensitive types of pain receptors in the body.
How it happens: Some post-op pain should be expected after an implant, but it’s usually less than the pain of having a tooth pulled.
How to fix it: This type of pain after a dental visit should go away without any sort of intervention. Just be aware of this before your implant, and call your dentist if the pain persists for more than a few days.
How long should dental implant pain last? Dental implant pain usually lasts about 2-3 days.
What it is: If you have receding gums that have progressed to exposing sensitive dentin (or bone), your dentist may suggest you have gum graft surgery.
What it feels like: Pain after gum graft surgery can be significant, with a combination of bone pain and gum pain in two different parts of the mouth. Expect the pain to be generalized and somewhat severe for several days.
How it happens: In gum graft surgery, your gums are purposefully “injured” in the process of correcting gum recession. Because dentin was exposed, you’ll also have bone pain as a result of increased contact between dental instruments and bone.
How to fix it: This pain should be expected after gum graft surgery. Your oral surgeon should recommend pain relievers or give you a prescription for one. Let him or her know if the pain lasts longer than a week and doesn’t subside.
How long should gum graft surgery pain last? Gum graft surgery pain typically lasts a week or less.
What it is: Trismus is a spasm of the jaw muscles, causing the mouth to remain tightly closed.
Trismus is sometimes called lockjaw, although it’s not the same “lockjaw” as a tetanus infection.
What it feels like: With trismus, your jaw muscles will spasm and close the mouth tightly. You can expect pain from the tensed muscles and possibly some tooth sensitivity from grinding.
Soreness and tenderness in the lower jaw are also symptoms of trismus.
How it happens: The needle used to inject local anesthetic may go through the muscle when a dentist is working on your lower teeth.
This doesn’t usually produce pain immediately following the procedure. But in 2-3 days following the procedure or injection, the muscle may stiffen, making it hard to open your mouth.
The condition will always be on the same side as the injection site, but it is fairly rare. You could also have it on both sides if you’re having your wisdom teeth out, though that’s even more rare.
How to fix it: Trismus is a condition your dentist should help you treat. He or she may prescribe a soft foods diet, physical therapy or massage, a jaw-stretching device, and/or muscle relaxers and pain relieving medication.
How long should trismus last? Trismus should last 2 weeks or less.
What it is: Tooth sensitivity may happen after dental procedures like a teeth cleaning or even a dental crown . Anytime tooth enamel or gums are worked on, sensitivity can result.
What it feels like: Tooth sensitivity is generalized soreness when teeth are exposed to very hot or very cold foods or drinks.
How it happens: Tooth sensitivity is a normal pain to expect after any dental procedure. It happens because the sensitive tissues of the teeth and gums have been agitated during normal dental care.
This is more likely during a root planing and scaling , a deep teeth cleaning performed during gum disease treatment.
In some cases, a dental filling is too high and can cause sensitivity (usually on just one side of the mouth).
How to fix it: Tooth sensitivity from a dental procedure should go away on its own, but you can try a salt rinse or benzocaine for relief. If you know you struggle with sensitivity after normal procedures like cleanings at your check-ups, try tips for making your cleanings less painful .
If you got a dental filling that is too high and interferes with your bite, you’ll need to go back to the dentist to resolve the sensitivity.
How long should tooth sensitivity last? Tooth sensitivity caused by dental work should go away in 2-3 days.
While some pain is to be expected after most dental procedures, there are a few steps you can take to prevent it before it starts.
To prevent pain after dental work:
- Eat an anti-inflammatory diet. Eating anti-inflammatory foods before you go to the dentist can be helpful in reducing how much pain you experience afterwards.
- Treat your TMD/TMJ before any procedure. If you’re more susceptible to jaw pain, try giving your muscles some light stretching and more rest before you go into a dental procedure.
- Ask for a bite block. To give your jaw muscles a break, you can request a bite block be used during your procedure to minimize muscle pain afterwards.
- Deal with bruxism (grinding) issues before your procedure. Grinding your teeth is likely to trigger pain after dental work. Treating that ahead of time will go a long way in helping you have a quick recovery.
- Deal with infection before having a cavity restored. Your doctor may give you antibiotics before having a root canal or dental filling . The less infection and smaller the abscess near a cavity, the less pain you’re likely to experience after having it fixed.
- Ask for a break in the middle of a long procedure. If your mouth has to be opened wide for several hours, asking ahead of time for a break in the middle is one way to prevent extra jaw muscle pain.
- Relax! Stress can cause a number of pain-inducing conditions like dental anxiety, muscle aches, and even some extra tooth grinding. Practice mindfulness and rest in the days leading up to your procedure. You might even try some CBD for dental anxiety if you know you’re nervous before your dental work. Using weighted blankets, noise-canceling headphones, or working with a therapy dog helps to provide some calm from the anxiety that many people feel before dental work.
Prevention is always your best tool for preventing tooth pain. In general, a large majority of dental work can be avoided by addressing dental health on a regular basis.
To prevent dental problems that require restorative procedures:
- Practice good oral hygiene. Use an electric toothbrush , a remineralizing toothpaste , and scrape your tongue at least twice every day. Never skip flossing. Good oral care is key to good oral health!
- Eat a tooth-friendly diet . Foods can cause or prevent/reverse cavities . Focus on nutrient-dense foods with minimal processing, sugar, and acid content.
- Don’t ignore signs of periodontal disease. Gum disease is incredibly common, especially after the age of 60. It’s associated with dozens of comorbid health conditions — don’t ignore it. Talk to your dentist about bleeding gums .
- See your dentist every 6 months. Dental health care is a huge part of your overall health. Bi-yearly dental appointments are important because teeth cleanings and regular exams can prevent small problems before they become big.
- Address sleep-disordered breathing . Sleep-disordered breathing (SDB), like that seen in sleep apnea, is a problem for countless reasons — one of which is poor oral health. SDB is associated with bad breath , TMJ, and weakened tooth enamel, among other issues.
For pain relief after dental work:
- Eat an anti-inflammatory diet. A diet high in plant-based foods , essential fatty acids, high-antioxidant foods, and foods with plenty of trace minerals reduce all-body inflammation . Inflammation is the root cause of most pain. Popular anti-inflammatory diets include the keto diet , Paleo diet, Mediterranean diet, or Whole30.
- Try a turmeric supplement. Turmeric is one of nature’s most potent natural pain relievers . Turmeric even outperforms some non-steroidal anti-inflammatory drugs used for pain and may treat postoperative pain.
- Rest and ice your jaw. If TMJ pain is your biggest issue, do what you can to relax your jaw before and after the procedure. Use an ice pack to reduce swelling and calm muscle inflammation. Avoid having dental work performed at a dental school , as the procedures done there usually take longer.
- Try THC or CBD. Both major compounds in marijuana, THC and CBD, are powerful pain relieving agents .
- Drink ice-cold coconut water. Coconut water can help to replenish electrolytes that you may lose during wisdom teeth removal recovery . Drinking it ice cold may reduce inflammation and soft tissue pain.
- Take an over-the-counter painkiller like ibuprofen. Ibuprofen is generally considered the best pain reliever for tooth pain . You may also try acetaminophen (Tylenol). I recommend patients follow the 3-3-3 method: 3 ibuprofen, 3 times a day, for 3 days after dental work.
- Take pain medications prescribed by your dentist. Opioids like Tylenol-3, Vicodin (Lortab; acetaminophen with hydrocodone), and Percocet (acetaminophen with oxycodone) may be used for dental pain. These are not prescribed as often as they used to be due to the opioid epidemic. Your dentist is unlikely to prescribe these pain medications except in extreme cases.
Should my teeth hurt after a cleaning?
Your teeth may be sore or sensitive after a cleaning. The longer it’s been since your last cleaning, the more likely it is you’ll have soreness.
If you’ve waited years to get a cleaning, your hygienist might need to do a full scaling and root planing to clear your teeth of plaque.
After that, your roots will be very clean — but they’ll be sensitive to cold for 1-2 weeks.
Very healthy teeth and gums that are regularly cleaned probably won’t hurt after a cleaning, although a bit of gum soreness for a day or two is normal.
Is it normal to have tooth pain after a filling?
After a filling, some pain is normal. Usually, you’ll notice soreness around the tooth for 1-2 days.
Metal fillings tend to cause pain more easily than plastic fillings, but plastics can cause pain in their own way, too.
There are two types of pain from a filling that would send you back to the dentist, though.
Aching and cold sensitivity around a filled tooth that lasts more than 3 days may be a sign of pulpitis. Pulpitis can be reversible or irreversible. The latter would, unfortunately, require a root canal or tooth extraction.
That’s why you should always get cavities filled once they’re small but have passed the point of reversal. The larger the cavity, the bigger your chance to develop pulpitis.
The second reason a filling could cause pain longer than a couple of days is a filling that’s too high. A tall filling may mess with your bite.
How do you know this has happened? You’d notice cold sensitivity and some aching about 2-3 days after getting the filling, and the pain would not get better over time.
Both of these reasons for tooth pain after a filling will send you back to the dentist for some type of correction.
How do you know if you have an infection after dental work?
Infections after dental work may cause:
- Bad taste in the mouth
- Toothache or new hot/cold tooth sensitivity
- Gum swelling
- Swollen jaw
- Swelling of the lymph nodes or neck
If you think you have developed an infection after dental work, talk to your dentist immediately.
- Watzl, B. (2008). Anti-inflammatory effects of plant-based foods and of their constituents. International journal for vitamin and nutrition research, 78 (6), 293-298. Abstract: https://pubmed.ncbi.nlm.nih.gov/19685439/
- Chrysohoou, C., Panagiotakos, D. B., Pitsavos, C., Das, U. N., & Stefanadis, C. (2004). Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults: The ATTICA Study. Journal of the American College of Cardiology, 44 (1), 152-158. Abstract: https://pubmed.ncbi.nlm.nih.gov/21139128/
- Sun, J., Chen, F., Braun, C., Zhou, Y. Q., Rittner, H., Tian, Y. K., … & Ye, D. W. (2018). Role of curcumin in the management of pathological pain. Phytomedicine, 48 , 129-140. Abstract: https://pubmed.ncbi.nlm.nih.gov/30195871/
- Takada, Y., Bhardwaj, A., Potdar, P., & Aggarwal, B. B. (2004). Nonsteroidal anti-inflammatory agents differ in their ability to suppress NF-κB activation, inhibition of expression of cyclooxygenase-2 and cyclin D1, and abrogation of tumor cell proliferation. Oncogene, 23 (57), 9247. Abstract: https://pubmed.ncbi.nlm.nih.gov/15489888/
- Agarwal, K. A., Tripathi, C. D., Agarwal, B. B., & Saluja, S. (2011). Efficacy of turmeric (curcumin) in pain and postoperative fatigue after laparoscopic cholecystectomy: a double-blind, randomized placebo-controlled study. Surgical endoscopy, 25 (12), 3805-3810. Abstract: https://pubmed.ncbi.nlm.nih.gov/21671126/
- Mack, A., & Joy, J. (2000). MARIJUANA AND PAIN . Full text: https://www.ncbi.nlm.nih.gov/books/NBK224384/
- Bailey, E., Worthington, H. V., van Wijk, A., Yates, J. M., Coulthard, P., & Afzal, Z. (2013). Ibuprofen and/or paracetamol (acetaminophen) for pain relief after surgical removal of lower wisdom teeth. Cochrane Database of Systematic Review s, (12). Full text: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004624.pub2/full
About Mark Burhenne, DDS
I’m on a mission to empower people everywhere with the same evidence-based, easy-to-understand dental health advice that my patients get. You can read my story here. I have been a dentist in private practice for 35 years. I graduated from the Dugoni School of Dentistry in San Francisco, CA in 1987 and am a member of the American Academy of Dental Sleep Medicine (AADSM), Academy of General Dentistry (Chicago, IL), American Academy for Oral Systemic Health (AAOSH), and Dental Board of California.

Dr. Mark is the author of the best-selling book 8-Hour Sleep Paradox
Jaw Pain 2 Weeks After Dental Work: Understanding Post-Procedure Discomfort
Experiencing jaw pain two weeks after dental work can be concerning. While some discomfort immediately following a dental procedure is common, persistent pain after an extended period warrants further attention. It’s important to understand that this type of pain may be a sign of complications such as infection, damage to the jawbone or nerves, or an issue with the alignment of the bite.

Determining the underlying cause of jaw pain after dental work is crucial. If the pain is accompanied by swelling, fever, or general malaise, seeking medical advice is critical to prevent any serious complications. Even in the absence of these symptoms, it is wise to contact a dental professional to evaluate the situation. They can provide guidance on pain management techniques and, if necessary, additional treatments to resolve the discomfort.
Key Takeaways
- Persistent jaw pain after dental procedures should be evaluated by a professional.
- Proper diagnosis is key to managing and treating post-dental work jaw pain effectively.
- Maintaining oral health and prompt attention to potential complications can prevent further issues.
Understanding Jaw Pain After Dental Work

After undergoing dental work, it’s important for individuals to recognize that jaw pain is a possibility. My focus is to provide clear information on the common causes of this pain and how to identify its symptoms.
Common Causes of Post-Dental Work Pain
The causes of jaw pain following dental procedures are often multifaceted, involving a variety of factors:
- Muscle Strain: Extended periods of keeping the mouth open can lead to muscle strain, which I find is a frequent cause of discomfort after dental treatment.
- Inflammation or Swelling: Invasive procedures like oral surgery can provoke inflammation around the affected area, contributing to pain.
- Dental Treatment: Specific treatments, such as a root canal or the placement of a blood clot after an extraction, may be associated with post-procedure ache.
- Trismus: Also known as “lockjaw,” this condition can result in a restricted ability to open the mouth fully and may emerge after certain dental work.
- Temporomandibular Joint (TMJ) Issues: I note that procedures can sometimes exacerbate underlying TMJ issues, leading to pain or discomfort.
- Injury to Bone or Soft Tissue: During dental work, accidental injury to the surrounding bone or tissues might occur.
- Infection: Post-procedure infections are potential causes of pain and should be addressed promptly by a dentist.
Identifying Symptoms of Jaw Pain
Symptoms associated with jaw pain may vary but commonly include:
- Aching Pain: This can occur continuously or during specific activities, such as biting or chewing.
- Swelling: Visible or palpable swelling in the area of the jaw.
- Stiffness: Difficulty in opening the mouth or a sensation of stiffness in the jaw muscles.
- Localized Tenderness: Pain is often felt at the site of the dental work or may radiate to surrounding areas.
- Changes in Bite: An altered bite can be a sign that there has been a change related to the dental procedure.
If symptoms persist, it becomes crucial to consult with a dentist to rule out more serious conditions or complications. They can provide an accurate diagnosis, which is key to determining the proper course of treatment for the pain.
Managing and Treating Jaw Pain
In the weeks following dental work, effectively managing jaw pain is crucial for recovery and quality of life. I’ll discuss immediate strategies for pain relief as well as long-term management techniques to prevent ongoing discomfort.
Immediate Pain Relief Strategies
To address jaw pain soon after dental procedures such as extractions or surgery, I use cold compresses to reduce swelling and soreness. Over-the-counter pain relievers like ibuprofen, which are anti-inflammatory, help to alleviate the immediate pain. When my patients complain of severe pain, I might recommend a course of prescription pain medication , ensuring to follow the American Dental Association’s guidelines. For those who have undergone procedures that may cause limited range of motion or lockjaw , a local anesthetic may be administered during the procedure, and I often suggest gentle jaw exercises to aid mobility.
Long-Term Pain Management and Prevention
For persistent jaw pain resulting from dental work or underlying conditions like TMJ disorder, my approach often involves a combination of physical therapy , jaw exercises , and possibly a nightguard or bite splint to prevent stress from teeth grinding. Anti-inflammatory medications and muscle relaxants can be used to manage muscle spasms . If there is sensitivity in the lower jaw or after procedures like a filling or tooth extraction, I may adjust the bite block used during the procedure or create a QuickSplint to facilitate healing. Regular check-ups are essential to monitor healing, prevent future dental problems , and adjust treatment as necessary. I work with my patients to develop tailored strategies that cater to their specific needs and conditions.
By remaining attentive to these strategies, I can manage my jaw pain effectively and prevent future complications stemming from dental work.
Potential Complications to Watch For
As a dentist, I recommend being vigilant for any signs of deviation from the expected healing process after dental procedures, particularly if you’re experiencing jaw pain two weeks post-procedure.
Recognizing Signs of Complications
Possible post-dental work complications can range from mild to severe. If you’re encountering persistent pain after dental work , it might be indicative of an infection or dry socket , a painful condition where the blood clot at the site of the tooth extraction fails to develop or dislodges. Sore jaws can signify jaw and muscle strain/sprain (JAMSS) , which is often a result of keeping the mouth open for extended periods during dental work. Occasionally, pain may not originate from the site of the surgery but can be referred pain from surrounding tissues.
- Infection : Watch for swelling , redness, bleeding , or discharge, as these are telltale signs.
- Abscess : A localized collection of pus indicates a bacterial infection, requiring prompt attention.
- Locking of the jaw or significant difficulty when opening or closing your mouth can be associated with TMJ disorders, which may be exacerbated by dental interventions.
When to Seek Further Dental or Medical Care
After dental work, if symptoms like pain or discomfort don’t improve, it is crucial to consider the following:
- Persistent Symptoms Beyond 2 Weeks : Ongoing or worsening pain, swelling, or jaw stiffness beyond the typical recovery timeline necessitates evaluation.
- Signs of Infection : Fever, pus, or swelling may indicate an infection. In such cases, antibiotics may be required.
- Severe Pain : Severe or escalating pain can be due to dry socket or other complications and should be assessed promptly.
- Periodontal Concerns : Excessive bleeding or signs of gum disease should be addressed to avoid damage to the periodontium.
- Unexplained Symptoms : Should you experience any unexpected symptoms like numbness or a bad taste in your mouth, ensure to seek an expert opinion.
Be mindful that factors such as aging can affect the healing process. Consistent with optimal dental care practices, follow your dentist’s post-operative instructions and don’t hesitate to report any concerns about your recovery.
Promoting Optimal Oral Health
Maintaining oral health is vital to avoiding jaw pain following dental procedures. I’ll guide you through daily routines and regular check-ups to ensure your jaw and dental health remain in top condition.
Daily Practices for Jaw and Dental Health
In my daily routine, I focus on thorough oral hygiene to prevent complications such as gum disease, which can lead to tooth sensitivity and orofacial pain. I use the following practices:
- Brush and Floss Regularly : Brushing twice a day with fluoride toothpaste and flossing once helps me keep my teeth and gums healthy.
- Limit Cold and Hard Foods : To avoid strain on my jaw, I minimize consumption of foods that are especially cold, hard, or chewy.
- Manage Stress : I practice stress-relieving techniques like deep breathing or yoga to prevent teeth grinding, known as bruxism, which can cause tenderness in the jaw muscles.
- Night Guards : If I experience bruxism, I consult my dentist about using an anterior bite splint to reduce teeth grinding while I sleep.
Routine Dental Care and Check-Ups
Regular visits to the dentist are crucial. Here’s how I maintain this routine:
- Regular Dental Examinations : I schedule visits every six months to check for health conditions that may affect my oral health, including the state of my temporomandibular joint (TMJ), which connects my jawbone to my skull.
- Cleanings : Professional cleanings help me prevent conditions like tenderness and stiffness in my jaw, which can escalate from gum disease.
- Addressing Dental Issues Promptly : If I experience symptoms like an earache or tooth sensitivity, I promptly seek my dentist’s advice to avoid complications like muscle strain or sprain from dental injuries.
- Pain Management : For minor jaw pain after dental work, I use recommended pain relievers like acetaminophen or aspirin, but always after consulting my dentist or doctor.
I incorporate these practices into my life, keeping my oral health in optimal condition and addressing potential issues promptly and effectively.
Frequently Asked Questions
I understand that experiencing jaw pain after dental procedures can be concerning. Here’s what you need to know about addressing this discomfort and seeking relief.
What treatments are available for jaw pain following dental procedures?
For jaw pain post-dental work, treatment options can include pain relievers, hot or cold compresses, and jaw exercises. In more severe cases, a dentist might recommend a mouth guard, muscle relaxants, or physical therapy.
Is it normal to experience difficulty opening my mouth due to jaw pain after dental work?
It’s not uncommon for patients to report difficulty opening their mouth due to jaw pain after dental work. This can often be attributed to muscle strain or inflammation and typically resolves within a few days to a week.
What could be causing persistent jaw pain months after undergoing dental work?
Persistent jaw pain months after dental work could be due to a variety of reasons such as temporomandibular joint (TMJ) disorder, an improperly placed filling or crown, or an unresolved infection. It’s crucial to consult with a dentist for a comprehensive evaluation.
Is pain at the site of a dental injection expected to persist for over a week?
Mild pain at the injection site is common and can last a day or two; however, if the pain persists for over a week, it may be indicative of tissue irritation or injury. Consulting a dentist is advisable if pain continues or worsens.
What are the potential causes of jaw pain specifically after receiving novocaine injections?
Jaw pain following a novocaine injection could result from the needle injuring tissues or the anesthetic causing temporary nerve inflammation. This discomfort is typically short-lived, but if prolonged, warrants a visit to the dentist.
How long is it typical for TMJ symptoms to last following dental work?
TMJ symptoms after dental work can vary in duration, but most people experience relief within a few days to a couple of weeks. Persistent or worsening symptoms should be evaluated by a healthcare professional.
Related Posts
- Gummies for Erectile Dysfunction: Uncovering the Benefits and Science
- Menopause Cold Flashes: Understanding and Managing this Uncommon Symptom
- Stomach Vagus Nerve Massage: Techniques for Digestive Health and Relaxation
- Why Are My Hands Always Cold: Uncovering the Common Causes
- Best Sleep Aid for Adults with Anxiety: Top Solutions for Restful Nights
- Polyphenol Rich Olive Oil: Unveiling Its Health Benefits
- How to Stop Being Gassy at Night: Effective Tips for a Peaceful Sleep
- Does Caffeine Affect Testosterone Levels: Unveiling the Truth

How Long Does Jaw Pain Last After Dental Work? (What To Do)
Have you ever woken up with a painful, uncomfortable stiffness in your jaw? The kind that feels like your jaw is so strained that you can’t open your mouth properly, and if you do, the mouth opening is way smaller than it usually is?
There are plenty of reasons why someone might suffer from soreness in their jaw. The many causes of jaw strain include having slept in a messed-up position overnight, or perhaps a bad habit of teeth grinding when you’re in a stressful situation.
But there’s one question you’re not asking yourself—did you have a dental procedure done in the last few days?
Dental work might be the reason why you’re feeling the symptoms of painful lockjaw. But why does it happen? And how long does jaw pain last after dental work? Today, we’ll answer all that and more.
Why Does My Jaw Hurt After Visiting the Dentist?

When you sit in the dentist’s chair with your mouth open for far too long, your jaw muscles will start to feel strained and overworked. This is especially common for oral surgery, a root canal, dental implants, or tooth extraction, which last longer than routine procedures like cleanings and fillings.
You won’t feel your jaw muscles being stretched out right away. It could take days after your appointment before you start feeling how fatigued your jaw is. The earliest sign of jaw strain from dental work is trismus, aka the feeling that your mouth can’t open as wide.
Discomfort and swelling in the jaw area after getting dental work done are likely due to temporary damage in your temporomandibular joint, also known as TMJ . This joint connects your skull to your jawbone. If it gets strained, it can be difficult to control your jaw’s muscles and how it moves.
A strain in your TMJ is more likely if a dentist treated a tooth in the back of your mouth. That’s because working further into your mouth requires you to open it wider for an extended period of time.
You wouldn’t strain your jaw the same way if your dentist was working on your front teeth, since it’s an area of your mouth that is easier to access.
Another reason why you could have jaw pain after a trip to the dentist is because of a dental injection . Some people find that the trauma of a local anesthetic via needle will be bothersome in the jaw area for a few days after their procedure.
How Long Does the Jaw Discomfort Last?
Once you start feeling the swelling and strain in your jaw, it may take a few days to around a week for it to feel normal again. The exact number of days before the discomfort goes away depends on several factors, such as your history with a previous TMJ disorder and your pain tolerance.
It also depends on the actual cause of the TMJ pain after you got dental work done. If it was caused by the dental injection, the pain and discomfort will likely go away in just two or three days. If you’re lucky, your jaw might even start feeling comfortable again just hours after your procedure.
But if the jaw pain is a result of keeping your mouth open for a long time, the stiffness may last longer. Give it around two days to a full week before you can expect to start feeling better.
If it doesn’t go away after a week, give your dentist a call so they can assess the situation and suggest ways for you to manage the pain until it’s gone.
How to Manage Jaw Pain Until It Goes Away

Patience is a virtue when waiting for the strain in your jaw to fade. But that doesn’t mean you should just sit and tolerate the pain. Here are some ways to manage the discomfort and relax your jaw muscles while you’re in the thick of it:
1. Rest your jaw and avoid straining it
Avoid straining your jaw even further by allowing it to get as much rest as possible. Don’t do things that will make your jaw exert too much effort, such as chewing gum, biting hard foods, and talking and laughing too much. These will aggravate your TMJ pain even more.
2. Do some jaw exercises throughout the day
Give your jaw a bit of physical therapy at home by doing simple exercises to stretch it out slowly but surely. Not only can it provide instant relief when your jaw feels extra tense, but it can also speed up the healing process.
Chin tucks and slowly opening and closing your mouth are easy and effective exercises you should do a couple of times a day to stretch your jaw muscles.
Need to stretch out your TMJ to help relieve it of tension after getting dental work done? Follow along with these exercises—they’ll be sure to give you some relief:
3. Massage your jaw joints with your fingers
When you wake up in the morning, fight the urge to open your mouth wide to yawn. It’s still sensitive. Before you do any activity that requires you to open your mouth, give it a five-minute massage with your fingers.
All you have to do is put your fingers near your jaw joints and then massage the area with circular motions. Apply gentle pressure only, nothing too hard or aggressive that can cause your jaw to swell even more.
4. Try hot or cold therapy
If your jaw is swelling and feels extra inflamed, experiment with hot and cold compresses to see which one works for you. Hot compress is amazing for relieving your muscles of stress and tension. Meanwhile, ice packs are super soothing for overfatigued muscles.
5. Manage it with over-the-counter pain medication
When all else fails and you still feel uncomfortable with the pain and stiffness in your jaw, take some pain medication. Look for anti-inflammatory meds like Ibuprofen and NSAIDs. You can also ask your dentist to prescribe you a muscle relaxer.
How to Prevent TMJ Pain After a Dentist Appointment

Next time you get a dental procedure done at the dentist’s office, communicate with them about your bad experience with jaw pain. Let them know which procedures resulted in that jaw stiffness.
For your succeeding appointments, your dentist will likely use a soft, cushiony bite block to prop your mouth open during your procedures. That way, there’s not a lot of strain from your jaw area to keep your mouth open. You can simply relax, and the bite block will keep your mouth open.
You can also prevent stiffness and pain later on by doing jaw exercises and massages as a preventive measure. That way, your jaws are stretched well and don’t hold in the tension from the dental procedures. Hopefully, the pain and stiffness will never come.
When Does Jaw Pain Become Worrisome?
Most of the time, jaw pain is only caused by injection trauma or straining your muscles in that area while getting dental work done. But sometimes, it could be a sign that there is something very wrong going on in your teeth or gums.
If the jaw pain doesn’t go away in a week and is starting to radiate to other parts of your body (like your neck and ear), you may have a dental abscess . This means there is a pocket of infectious pus in your gums or the bone holding your teeth together.
Other signs of a dental abscess include fever, headaches, earache, increased sensitivity to hot and cold food, and an unpleasant odor in your mouth.
If you suspect that you have a dental abscess, book an appointment with your dentist immediately. They’ll diagnose you properly and give you the right medication to treat the infection.
Jaw pain is also worrisome if you are in extreme, unbearable pain—the kind you lose sleep over because it hurts too much. This may be a sign that you have dislocated your jaw while getting dental work done. In this case, go to your dentist right away so they can check it out.
TMJ pain and inflammation are side effects of dental procedures that force you to strain your jaw and keep your mouth open for long periods. But don’t worry—this is completely normal. In a few days, your jaw and orofacial pain will subside fully, and you’ll be back in tip-top shape.
While you’re waiting for the muscle strain to run its course, do things to remedy the pain. Exercise your jaw, give it massages in the morning, and treat it with a hot or cold compress. And if you really can’t handle the discomfort anymore, you can always grab some over-the-counter pain meds.
Next time you go to the dentist, make sure to tell them about your jaw pain. Communicate it properly so your dentist knows to be extra careful and give you a bite block if they need you to open your mouth for a while. Hopefully, you don’t experience jaw pain again.
Related posts:
- How To Relieve Jaw Pain After Dental Work? (Causes And Treatments)
- How Long Does Dental Injection Site Pain Last? (Explained)
- How Long Does Dental Numbing Last? (Recovering Faster Tips)
- How Long Does It Take to Become a Dental Assistant?
- How Much Does A Dental Check Up Cost? (Ultimate Guide)
- How Much Does It Cost To Get A Full Mouth Of Dental Implants? (Average)
- How Much Does Dental Bonding Cost? (Average)
- How Much Does Dental Bridge Cost With Insurance? (An Estimate)
Similar Posts

Dental Hygienist VS. Dental Assistant: What To Expect When You Join
Being a dentist isn’t the only career path one can follow if they want to pursue dental…

How Much Is A Dental Checkup Without Insurance? (By States & Exam Type)
Dental services can be pricey nowadays, especially depending on where you live. That can be a problem…

How To Stop Dental Bone Loss? (Causes & Treatments)
Have you noticed the thinning of your dental bones? Are your teeth shifting and loosening from the…

Is Dental Insurance Worth It? (Pros & Coins)
Primary dental insurance is far less complicated than health insurance and has the purpose of helping you…

How Long is the Human Canine Tooth?
A Detailed Overview of Canine Teeth in Humans The canine teeth are a crucial part of the…

What is a Dental Emergency? (6 Types)
Usually, through correct dental hygiene practices and regular trips to see a dentist for check-ups, we can…
Jaw Joint and Muscle Strain/Sprain Treatment Technique
by Brad Eli, DMD, MS; James Fricton DDS, MS
Introduction One of the most common non-infectious complications resulting from dental care is jaw joint and muscle strain/sprain. Jaw joint and muscle strain/sprain are characterized by acute joint pain, limited range of motion, muscle tenderness, and muscle and joint dysfunction. If left untreated, these can progress into a chronic condition. This article presents a treatment technique for effectively managing 1st and 2nd degree jaw strain/sprain injuries and presents two cases demonstrating its use.
Jaw Joint and Muscle Strain/Sprain: A Common Complication from Dental Care Jaw joint and muscle strain/sprain can occur after lengthy dental procedures requiring opening the mouth wide or from forces placed on the jaw during dental care. Procedures such as mandibular blocks, crown preparation, dental extractions, periodontal, endodontic, etc., can cause jaw joint and muscle strain/sprain. Additionally, finger rests can place forces on the jaw and cause hyperextension of the joint and strain of the muscles. Acute jaw joint and muscle sprain/strain after dental procedures is more common than originally thought with more than 50% of patients with temporomandibular disorders (TMD) reporting their pain onset as a direct result of dental care.1-13 In one study of 164 patients with TMD, trauma was the initiating factor in 50.6% of cases, with 61% of these cases coming from trauma and strain during dental treatment.7 Among young adults, 23% of all jaw pain cases had their onset after third-molar extractions.8-9 Other causes of jaw trauma include motor vehicle accidents, intubation during general anesthesia, yawning, blows to the jaw, or hard and sustained chewing.10-13 Early Treatment Can Prevent Progression to a Chronic Condition When a jaw joint and muscle strain/sprain does occur, it is important to take appropriate early steps to encourage rapid healing to resolve pain and mitigate any risk factors that can delay recovery. These steps must include adequate treatment of the injury and reduction of complicating risk factors, such as parafunction, muscle bracing, and jaw overuse. Failure to provide prompt treatment can result in a progression to a chronic pain condition.
If pain is untreated, peripheral and central sensitization occurs due to the neuroplasticity of the nervous system and recruitment of agonist muscles.14 Local tissues become more tender and sensitive to mechanical stimulation. As the pain progresses to chronic, additional signs of sensitization including allodynia (sensitivity to normal touch) and hyperalgesia (more pain with normal stimulation) may develop. Initial symptoms can increase to include headaches, earaches, neck pain and jaw dysfunction such as clicking and locking. Since oral and facial structures are essential to eating, communication, and hearing, and strongly influence appearance, self-esteem, and personal expression, chronic orofacial pain can affect quality of life, functioning, emotional status, and dental care.
Treatment of Jaw Strain/Sprain Acute sprain/strains can occur at any joint and muscle group. Sprain/strains can vary from 1st degree (slight muscle or ligamentous tear with mild pain and functional limitation) to 2nd degree (partial muscle or ligament tear with blood clot formation, moderate pain, and functional impairment) and 3rd degree (total separation of the muscle or ligament with severe pain, loss of function and stability). Signs and symptoms of each include progressively increasing pain, tenderness, swelling, limited range of motion, and functional loss ( Fig. 1 ).

To encourage rapid healing of sprain/strain injuries in 1st- and 2nd-degree injuries, a MEAT Protocol including movement, exercise, analgesia, and treatment is recommended. The treatment of a 3rd-degree injury requires a RICE protocol including rest, ice, compression, and elevation. This article provides a reliable and effective MEAT protocol for treating 1st and 2nd degree injuries commonly seen in a dental practice.
As part of this protocol for jaw injury, an interim anterior bite splint (night-time wear) should be used to support, relax, and protect the jaw joints and muscles, similar to how an elastic bandage supports and protects a wrist or ankle injury. Additionally, jaw exercises are prescribed to restore normal function and range of motion.
Jaw Joint and Muscle Strain/Sprain Treatment Technique This is a simple and effective treatment technique for patients who experience acute jaw pain after procedures. Much as in orthopedics, prompt treatment, preferably on the same day, improves success in reducing pain and dysfunction at the acute stage. Failure to provide treatment promptly can directly effect the outcome.
The four steps of the MEAT approach for 1st and 2nd degree jaw injuries include: 1. Movement . This includes self-care training in the proper use of the jaw and avoiding risk factors that can delay recovery. With 1st or 2nd degree injuries, a MEAT protocol and careful use of the jaw increases blood flow, encourages healing, and restores jaw function. Risk factors such as parafunction, muscle bracing, and jaw overuse should be avoided.
2. Exercises. Restoration of normal function can be achieved with exercises that focus on stretching to restore normal range of motion. In addition, posture and relaxation exercises reduce strain to the muscles and encourage healing. Patient jaw exercise instructions are available in notepad form for distribution (Jaw-Rx-ercises, QuickSplint LLC). Patients with chronic baseline conditions may also find self-help on-line training programs such as the International MYOPAIN Society (www.preventingchronicpain.org).
3. Analgesia . For pain relief, acetaminophen, anti-inflammatories, topical, or hydrotherapy (alternating heat and cold) reduce pain and facilitate movement, exercise, and healing. For more intense pain, the Center for Disease Control has developed opioid prescribing guidelines and provides a comprehensive user guide. Failure to provide adequate pain control can limit the patients’ willingness to move and can have a negative effect on outcome.
4. Treatment . The QuickSplint (QuickSplint LLC) is an immediate anterior bite splint that can be placed on the same day at chairside to help protect the jaw and is similar to a protective elastic bandage for ankle and wrist injuries. The splint, worn at night, can reduce jaw closing muscle activity (e.g., jaw clenching or tooth grinding), inhibits the maximum bite force, and helps to encourage healing of acute temporomandibular pain and related restricted jaw opening. The flat occlusal surface allows the mandible to move freely instead of closing into a specific dental relationship, and encourages healing and normal function. The advantages over traditional lab-manufactured splints include; 1) immediate placement (no impression), 2) custom fit, 3) large enough to avoid aspiration or swallowing, and 4) temporary (up to four weeks) to minimize occlusal changes and allow time to place a long-term splint ( Fig. 2 ).
FIGURES 2-5. QuickSplint is an immediate anterior bite splint that can be placed immediately at chairside to help protect the jaw and is similar to a protective elastic bandage commonly used for an ankle or wrist injury. QuickSplint is an immediate anterior bite splint that can be placed immediately at chairside to help protect the jaw and is similar to a protective elastic bandage commonly used for an ankle or wrist injury.

Case Study: Jaw Muscle Strain After Crown Preparation History of Present Illness : A 62-year-old female with no prior signs of parafunction, jaw symptoms or other health conditions presented a one-week history of sudden onset pain after crown preparation and placement on tooth 37. At onset, the patient was given a soft mouth guard. It was unsuccessful in treating her pain. The patient avoided chewing on her left side. Due to increased jaw dysfunction and her failure to improve after using a “soft splint,” she was referred to an orofacial facial pain (OFP) specialist.
Clinical Examination by the OFP Specialist Limited jaw opening measured 10 mm without pain extending to 28 mm with pain. Left jaw pain and headache; recent onset left eye and ear pain as well. Protrusive movements were within normal limits.
Assessment/Differential Diagnosis 1. Sprain and strain, left temporomandibular joint and associated muscles. 2. Possible disc displacement without reduction 3. R/O temporal arteritis Treatment Given the age of the patient, the risk of temporal arteritis is of concern. Sed rate would be indicated and was discussed with the patient, however, with the known onset and other differential diagnosis present, this blood test was placed on hold but informed consent was discussed. Regarding the possible disc displacement and possible “closed lock” based on the protrusive range, muscle guarding was thought likely and confirmed with spray and stretch that demonstrated 45 mm of opening. The primary diagnosis for treatment was sprain/strain of the medial pterygoid with likely post injection injury to the muscle. The patient was given an anterior overnight bite splint and educated on self-care measures that included jaw exercises for daytime use (MEAT protocol).
Results and Follow-Up The patient was seen two weeks later and reported a significant improvement. Due to prompt treatment and negative prior history, this patient demonstrated the orthopedic nature of the temporomandibular joint complex and its healing abilities. The condition resolved at the four-week follow-up. The patient confirmed that interim splint and the jaw exercises were helpful in resolving her condition.
At four weeks, wear marks consistent with significant parafunction were noted on the surface of the QuickSplint interim splint. This finding supports the lack of response to the original soft device. Use of soft “night guards” in the presence of significant parafunction is not recommended as it can aggravate the behavior in some patients. With this finding the patient was advised that she would benefit from tooth structure protection in the form of a hard, flat plane, full arch device with cuspid guidance.
Case Study Two: Pain After Bilateral Root Planing and Scaling Procedure History of Present Illness A 67-year-old male had bilateral scaling and root planning with anesthesia. During the two one-hour sessions, one-week apart, the patient’s jaw was open most of the time. One week following the second procedure, the patient experienced a sudden onset of pain with limited jaw opening.
Medical history was negative for risk factors; no prior history of TMJ problems or facial muscle pain. He was seen by the treating dentist who recorded a 22 mm painful jaw opening. No “pre-treatment” jaw range of motion (ROM) was recorded.
Due to his sudden onset of pain and significant limitation of mobility, the patient was provided anti-inflammatory and pain medication along with a referral to an orofacial pain specialist.
Clinical Examination by the OFP Specialist Two weeks from onset, the OFP examination was significant for limited ROM and pain. Maximum range of motion 24 mm with a hard end feel. No risks on medical history for muscle problems and no prior history of TMJ issues.
Differential Diagnosis Internal derangement bilateral TMJ without reduction (closed lock). Muscle splinting/guarding medial pterygoid bilaterally.
Treatment The patient was advised to wear the QuickSplint interim splint at night and part of the day. He was given daytime avoidance exercises (Jaw Rx-ercises) limited to pain-free range and alternating hot/cold pack for 30 minutes/day while watching TV or reading to improve blood flow. Hot and cold drinks were also recommended for better access to the medial pterygoid.
Results and Follow-Up At four weeks from onset, the patient’s muscle spasm had resolved. Jaw opening measured 45 mm without pain; the patient was advised to hold back on full jaw function for an additional two weeks. Due to prompt treatment and negative prior history, the patient demonstrated the orthopedic nature of the temporomandibular joint complex and its healing abilities. Discussion Jaw joint and muscle sprain/strain are common complications from dental care. The two cases are characteristic of common events. Prompt treatment, preferably on the same day, improves success in reducing pain and dysfunction at the acute stage, and, even more importantly, helps to prevent chronic pain. Failure to identify and treat jaw joint and muscle sprain/strain immediately can have a significant negative impact on prognosis, regardless of diagnostic prowess or expertise, and everything to do with the CNS and its response to unremitting pain. Within the dental profession, there are few clinical techniques related to treatment of jaw joint and muscle sprain/strain, and even less recognition of the prevalence of injuries, patient risk factors, and associated preventative measures. Treatment technique is improving due to the growing number of practitioners and researchers in orofacial pain. The treatment technique outlined in this article is designed to assist dentists in reliably providing conservative and appropriate care if a jaw injury occurs. OH
Bradley Eli, DMD, MS is a Board Certified Specialist in orofacial pain, TMD and related headaches. He developed the jaw joint and muscle strain/sprain treatment protocol and the QuickSplint for his own practice to treat patients suffering with acute jaw joint and muscle sprain/strain. James Fricton, DDS, MS is Professor Emeritus, University of Minnesota Schools of Dentistry, Medicine, and Public Health, Senior Investigator for HealthPartners Institute for Education and Research, and Pain Specialist at the Minnesota Head and Neck Pain Clinic. He is the President of the International Myopain Society. Disclosure : Orofacial pain specialist, Dr. Bradley Eli, is founder of QuickSplint LLC and has a financial interest in a product mentioned in this article. Oral Health welcomes this original article. References 1. Fricton, J., Kroening, R., Haley, D., Siegert, R.: Myofascial pain and dysfunction of the head and neck: A review of clinical characteristics of 164 patients. Oral Surgery, Oral Medicine, and Oral Pathology, 1985; 60(6):615-23.
2. Contar CM, de Oliveira P, Kanegusuku K, Berticelli RD, Azevedo-Alanis LR, Machado MA. Complications in Third Molar Removal: A retrospective study of 588 patients. Med Oral Patol Oral Cir Bucal 2009;15:74-8.
3. Huang GH, Rue TC. Third-molar Extraction as a Risk Factor for Temporomandibular Disorder. J Am Dent Assoc. 2006;137:1547-54.
4. Sahebi S, Moazami F, Afsa M. Effect of lengthy root canal therapy sessions on temporomandibular joint and masticatory muscles. J Dent Res Dent Clin Dent Prospects 2010; 4(3):95-7.
5. Huang GH, Leresche L, Critchlow CW, Martin MD, Drang- sholt MT. Risk factors for diagnostic subgroups of painful temporomandibular disorders (TMD). J Dent Res 2002; 81: 284-8.
6. Poveda-Roda R, Bagan JV, Jimenez-Soriano Y, Fons-Font A. retrospective study of a series of 850 patients with temporomandibular dysfunction. Clinical and radiological findings. Med Oral Patol Oral Cir Bucal. 2009; 14:e628-34.
7. Stone J, Kaban LB. Trismus after injection of local anaesthetic. Oral Surg Oral Med Oral Pathol 1979; 48: 29–32.
8. Backland LK, Christiansen EL, Strutz JM. Frequency of dental and traumatic events in the etiology of temporomandibular disorders. Endodont Dent Traumatol1988; 4:182–185.
9. Stacy GC, Hajjar G. Barbed needle and inexplicable paresthesias and trismus after dental regional anesthesia. Oral Surg Oral Med Oral Pathol 1994;77: 585–586.
10. Martin MD, Wilson KJ, Ross BK, Souter K. Intubation risk factors for temporomandibular joint/facial pain. Anesth Prog. 2007; 54:109-14.
11. Pullinger AG, Seligman DA. Trauma history in diagnostic groups of temporomandibular disorders. Oral Surgery, Oral Medicine, and Oral Pathology. 1991, 71(5): 529–534.
12. Burgess J. Symptom characteristics in TMD patients reporting blunt trauma and/or whiplash injury. Journal of Craniomandibular Disorders: Facial & Oral Pain [1991, 5(4):251-257.
13. Haggman-Henrikson B, Rezvani M, List T. Prevalence of whiplash trauma in TMD patients: a systematic review. J Oral Rehabil. 2014,41(1):59-68.
14. Maixner W, Greenspan JD, Dubner R, Bair E, Mulkey F, Miller V, Knott C, Slade GD, Ohrbach R, Diatchenko L, et al. Potential autonomic risk factors for chronic TMD: descriptive data and empirically identified domains from the OPPERA case-control study. J Pain. 2011 Nov; 12(11 Suppl):T75-91.
RELATED ARTICLE: Stem Cells From Jaw Can Create and Repair Cartilage
RELATED NEWS

New Study Shows Oral Bacteria May Accelerate Pancreatic Cancer Development

Researchers are Using an App to Help Patients Face Their Dental Fears

Patients Open to Support from Their Dentist on Weight Management, Study Finds
Dental health resources to consider for children with cleft lips and palates, kanye west receives ‘experimental’ titanium dentures, beauty salons offering dental services worry fiji dentists, the american heart association launches healthy smiles, healthy hearts™ initiative, tooth decay increasing for eastern ontario children, causing concern, australian dentist bringing smiles to people with special needs, dentist shortage linked to rise in oral cancer deaths, claims dental campaigners, surgical obesity treatment shown to increase risk of dental caries, diabetes patients can use special mouth rinse to help treat gum disease.

Women in Oral Health Care 2023

Technology: Today & Tomorrow

HPV-Related Head and Neck Cancers. Meet the Authors.

Life Can Throw You a Curve. Be Prepared by Planning Your Transition Now!

How to Cultivate a Culture of Safety in Your Dental Practice

How to Market this In-demand Service: Botox® and Other Injectable Treatments

Weekly Wisdom: Updating Your Employment Agreements

Weekly Wisdom: Restoring Endodontically-Treated Teeth

Weekly Wisdom: The Toughest Part of Selling Your Practice
We use cookies to make your website experience better. By accepting this notice and continuing to browse our website you confirm you accept our Terms of Use & Privacy Policy .
read more >>
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Complications After Dental Treatment
, DDS, Veterans Administration
More Information
Complications after a dental procedure that include swelling and pain, dry socket, osteomyelitis, bleeding, and osteonecrosis of the jaw comprise another set of urgent dental problems Introduction to Urgent Dental Problems Certain dental problems require prompt treatment to relieve discomfort and minimize damage to the structures of the mouth. Such urgent dental problems include Toothaches Fractured, loosened... read more that require prompt attention.
Swelling and pain
Swelling is common after certain dental procedures, particularly tooth removal (extraction) and periodontal surgery. Holding an ice pack—or better yet, a plastic bag of frozen peas or corn (which adapts to the shape of the face)—to the cheek can prevent much of the swelling. Ice therapy can be used for the first 18 hours. Cold should be held on the cheek for 25-minute periods every hour or two. If swelling persists or increases after 3 days or if pain is severe, an infection may have developed, and the person should contact the dentist.
Pain after a dental procedure can be moderate to severe. People can take various pain relievers.
Dry socket (alveolitis)
A dry socket (exposure of the bone in the socket, causing delayed healing) may develop after a lower back tooth has been extracted and the normal blood clot in the socket is lost. Typically, discomfort lessens for 2 or 3 days after the extraction and then suddenly worsens, sometimes accompanied by an earache. Although the condition goes away by itself after 1 to 2 weeks, a dentist can place a dressing soaked with an anesthetic in the socket to eliminate the pain. The dentist replaces the dressing every 1 to 3 days until no more pain is felt after the gauze has been left out for a few hours. Alternatively, dentists often use a commercial dressing that does not need to be removed and that contains an antimicrobial and a pain reliever in addition to an anesthetic. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be taken by mouth if additional pain relief is needed.
Dry sockets are much more common among people who smoke. If at all possible, people should not smoke for several days before and after the extraction is done. Women (especially those taking oral contraceptives) also have a high rate of developing dry socket.
Osteomyelitis
Osteomyelitis Osteomyelitis Osteomyelitis is a bone infection usually caused by bacteria, mycobacteria, or fungi. Bacteria, mycobacteria, or fungi can infect bones by spreading through the bloodstream or, more often, by... read more is an infection of the bone and is usually caused by bacteria. When osteomyelitis occurs in the mouth, it typically occurs as an infection of the lower jaw. People usually have a fever, and the affected area is tender and swollen. Doctors or dentists use an x-ray to make the diagnosis. People with osteomyelitis need to take antibiotics for an extended period of time.
Osteonecrosis of the jaw
Osteonecrosis of the jaw Medication-Related Osteonecrosis of the Jaw (MRONJ) Medication-related osteonecrosis of the jaw (MRONJ) is a rare and potentially debilitating condition that involves exposure of the bone of the jaws. MRONJ occurs in some people who have taken... read more is a disorder that involves bone death of areas of the jawbones after exposure of the jawbone through the gum tissue. The disorder usually causes pain, loosening of teeth, and a discharge of pus. The disorder may occur after
Tooth extraction
Radiation therapy to the head and neck (osteoradionecrosis)
Use of bisphosphonate drugs in high doses or for long periods

Treatment typically involves scraping away some of the damaged bone (debridement), taking antibiotics by mouth, and using antibacterial mouth rinses.
Bleeding after a tooth is removed is common. Bleeding in the mouth may appear worse than it is because a small amount of blood may mix with saliva and appear to be more blood than is actually present. Usually, the bleeding can be stopped by keeping steady pressure on the surgical site for the first hour, normally by having the person bite down on a piece of gauze. People may have to repeat the process two or three times. Keeping the gauze (or a tea bag) steadily in place for at least an hour is important. Most problems with bleeding occur because the person frequently removes the pack to see whether the bleeding has stopped. If bleeding continues for more than a few hours, the dentist should be notified. The dentist may need to clean out the bleeding area and surgically close it with stitches (sutures).
People who regularly take an anticoagulant (a drug that prevents clots) such as warfarin or aspirin (even if they take only one aspirin every few days) should mention it to the dentist a week before surgery because these drugs increase the tendency to bleed. The person’s doctor may adjust the drug dosage or temporarily stop the drug a few days before surgery after consultation with the dentist.
The following English-language resource may be useful. Please note that THE MANUAL is not responsible for the content of this resource.
Mouth Healthy: This resource provides information on oral health, including nutrition and guidance on selecting products that carry the American Dental Association's seal of approval, as well as advice on how to find a dentist and when to see one.
Drugs Mentioned In This Article

Was This Page Helpful?

Test your knowledge
Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada)—dedicated to using leading-edge science to save and improve lives around the world. Learn more about the Merck Manuals and our commitment to Global Medical Knowledge .
- Permissions
- Cookie Settings
- Terms of use
- Veterinary Edition

- IN THIS TOPIC

Jaw Pain After The Dentist
Persistent jaw pain after the dentist is something to take seriously. While local inflammation of the gums, soreness of the jaw muscles, and tooth sensitivity can be normal in the days after a dental procedure, prolonged jaw pain for more than a week could be indicating an injury to the temporomandibular joint (TMJ). Prolonged jaw pain is a serious issue because untreated jaw pain is a risk factor for the development of chronic TMJ pain disorders.
Here we cover the mechanics of jaw injury during dental work and then provide a plan for jaw pain relief.
There are several features of dental procedures that make the TMJ complex vulnerable to injury. To understand this, it helps to remember that the TMJ and its surrounding muscles and ligaments are one of the most complicated and most used joint systems in the body. The joint has two distinct planes of motion, a floating articular disc, major and minor ligaments, and four paired muscles that work together to accomplish the tasks of eating and speaking.
Just like any complex joint in the body, the jaw joint is vulnerable to sprain and strain injuries (called “jaw and muscle sprain/strain”, or JAMSS). Jaw sprain or strain can occur during dental work because of hyperextension of the jaw. When the dentist asks you to “open wide”, you open to your maximal comfortable distance, which for most people is around two fingers wide. But when instruments and hands are in the mouth, the jaw is often pushed beyond this comfort limit.
Jaw hyperextension can cause trauma to the TMJ ligaments and muscles, leading to a guarding reflex, where the muscles begin to contract and become tense. Strain injuries are most clearly documented in third molar removal cases, where there is often substantial force placed on the jaw, or where forced extension is used to get access to the back molars.
Prolonged dental procedures are also a problem. Even when the jaw is not hyperextended but is merely opened for long periods of time, it can trigger a guarding reflex in the jaw muscles. Recent studies have documented that a significant number of people having routine dental procedures that last over two hours can experience TMJ pain a week or more after the procedure. If you plan to have a long dental procedure, ask your dentist to give you a break somewhere in between to avoid this.
One final and confounding source of TMJ pain after the dentist is trauma from the injection of local anesthesia. Symptoms of injection trauma are usually limited to the first several days after the procedure and typically present as numbness and tingling rather than soreness and pain.
From Jaw Strain To TMJ Disorders
The guarding reflex in the jaw muscles is the common result of the above mechanisms of injury. This muscle hyperreactivity is the bridge between acute injuries and chronic TMJ pain. Here’s how it works:
- Persistent muscle tension after a strain injury leads to decreased oxygenation, muscle fatigue, and more pain.
- Soon, routine use of the jaw during eating or mouth opening begins to trigger pain signals.
- When these pain signals are persistent, they induce a hyperexcitable state in the neurons of the central nervous system. This is called “central sensitization”.
- Now, even normal sensations in the TMJ region register as pain in the brain, leading to even more guarding, more fatigue, and more pain.
This is the vicious cycle of pain that occurs in chronic TMJ disorders. Even though the original injury might have been microtrauma to the ligaments, chronic muscle tension and central sensitization perpetuate the pain long after the ligamentous injury is healed.
“Strain injuries from dental procedures need to be taken seriously. Studies have shown that over 50% of people with chronic TMJ pain cite dental work as the initiating factor. The key to preventing chronic TMJ pain is to aggressively treat jaw pain in the acute phase, when it first starts”, explains Bradley Eli, DMD, MS, an orofacial pain specialist.
Jaw Pain Relief
The best way to achieve jaw pain relief is to use a comprehensive approach, using multiple tools that bring you towards your goal of pain relief. Here are the main components in a multimodal treatment approach for jaw pain:
- Jaw Rest : This is achieved by starting a strict soft food diet and avoiding anything hard or chewy.
- Jaw Exercises : Physical therapy of the jaw is a proven intervention for relieving jaw pain.
- Hot/Cold Therapy : Alternating heat and cold can bring significant pain relief to sore muscles. Heat will also increase tissue extensibility, leading to improved jaw range of motion.
- Pain Management : Self-directed pain management exercises (such as cognitive behavioral therapy) can be powerful tools for helping to relieve pain. Over the counter analgesics can also be helpful.
- Oral Splint Therapy : Overnight use of an anterior bite guard (like the QuickSplint® ) can help unload tense jaw muscles and provide rapid relief to fatigued, sore muscles.
All of these interventions are included in the Speed2Treat® Home Healing Kit . The kit was designed by orofacial pain specialists to give you everything you need to comprehensively treat acute jaw pain. Don’t let your jaw pain turn into a chronic TMJ pain condition. Start your journey toward jaw pain relief today with the Speed2Treat® Home Healing Kit!
More Articles


Can Bruxism Cause Headaches?

New Jaw Pain After Dental Injection

What’s the Best Mouth Guard for TMJ Pain?

Why Do SSRIs Cause Jaw Clenching?
Applications, provider directory.
- Find a Provider
- Teledentist Consult
- List Your Practice
Subscribe to our emails
- Enter Your Email *
- Email This field is for validation purposes and should be left unchanged.
- Privacy Policy
- Terms of Use
- Medical Disclaimer
Information
- 800-760-0526
- Home Healing Kit
- QuickSplint
- Practice Aids
- Patient Aids
- Distributors
- Practice Tips
- Name This field is for validation purposes and should be left unchanged.
- Policy Privacy

Are You Provider or Consumer?

Inspiring Wellness, One Smile at A Time

TMJ after Dental Work: How Dental Procedures Can Impact Jaw Function
If you’re someone who struggles with a temporomandibular joint (TMJ) disorder, you may have experienced a flare-up in your TMJ after dental work . That’s because certain dental procedures , including common ones like routine cleanings, can cause irritation to the jaw and the area around it. Depending on the extent of that irritation – and the extent of your TMJ – the result could be a TMJ flare-up that requires a bit of extra care and attention in the hours and days after seeing your dentist.
TMJ is a disorder that affects the joints of the jaw, as well as surrounding muscles and ligaments. While symptoms do tend to come and go, flare-ups can be quite debilitating, and it makes sense that you’d be wary of anything that may lead to discomfort.
Fortunately, while jaw pain after dental work is not uncommon, it’s also not totally untreatable. Here’s what to know about why your TMJ may be exacerbated by dental work – plus helpful tips for feeling better.
Why You May Experience a TMJ Flare-Up After Dental Work
The connection between dental work and TMJ has less to do with the procedures themselves and more to do with the position your mouth is in while they happen.
In order to access your teeth and gums, a dental specialist needs you to keep your mouth open wide for a long period of time. It’s this sustained movement that can lead to a TMJ flare-up , since it requires the jaw muscles to work overtime. Depending on the procedure, you may also experience oral and/or facial inflammation that leads to further worsening of your TMJ symptoms.
Some of the most common TMJ symptoms you may experience after dental work include:
- Pain and/or pressure in the jaw, face, ears, or neck
- Jaw stiffness
- Jaw popping and clicking
- Difficulties opening and closing the jaw
- Locking of the jaw joints
- Hissing or ringing sound in the ears
- Pain behind the eyes
So, how long does TMJ take to heal on its own? Left untreated, TMJ symptoms will generally resolve within a few hours after dental work, though some people may experience symptoms that last for several days – or even weeks. The length of time it takes for TMJ symptoms to clear up depends on a number of factors, including how bad your TMJ pain is, the underlying cause of the disorder, and any current treatment methods you might be using.
Tips to Prevent Jaw Pain After Dental Work
If you are prone to extensive TMJ flare-ups, talk to your dentist ahead of any scheduled procedures so that they can try to accommodate your condition and reduce the risk of sustained discomfort.
Your dentist may recommend taking regular breaks during cleanings or other procedures to allow your jaw to rest. They may also give you opportunities to massage and stretch your jaw joints, which could prevent a flare-up of TMJ or reduce its severity.
Stress and anxiety can play a role in post-dental work jaw pain, too. That’s because the more stressed we are, the more we tend to grind and clench our teeth (a condition called bruxism). You can help reduce dental-related stress through practices like deep breathing, meditation, and progressive muscle relaxation. Many people also find it helpful to distract themselves during dental procedures by listening to music or audiobooks on headphones.
How to Treat TMJ After Dental Work and Feel Better Sooner
TMJ disorder is a tricky condition, and it’s not always possible to fully prevent it. But you can help yourself feel better by trying out one or more proven TMJ treatments.
Some of the ways to relieve the pain and discomfort of TMJ include:
- Applying heat or cooling packs to the affected area (heat is best for muscle soreness; cold will help address any inflammation)
- Taking over-the-counter pain relievers such as Tylenol or Motrin
- Eating soft foods and avoiding anything too crunchy, chewy, or sticky
- Gently massaging or stretching your jaw and/or neck (talk to your dentist for tips on how to do this safely)
- Wearing a mouthguard
It’s also a good idea to take steps to manage stress outside of the dentist’s office and prevent jaw clenching. Not sure where to start? Check out a guided meditation app on your phone, or simply set aside some time for general relaxation in the lead-up to a dental appointment.
See a Dentist About TMJ Pain
Don’t let fear of TMJ pain lead to you putting off important dental care and procedures.
Our team at Inspire Dental Wellness is committed to helping you manage your TMJ, whether it’s caused by dental work or is more of an everyday problem. We offer TMJ therapy that helps you get on the path to a pain-free life. We’ll also work with you to reduce stress before, during, and after your dentist appointment, and we can guide you on gentle movements that will mitigate the risk of jaw tightness following dental work.
Please contact us today to schedule an appointment at our clinic in Orland Park.
Terms and Conditions - Privacy Policy

Pain After a Dental Visit – What is Normal, What is Not?

You and I both know that Dental visits can be an absolute pain in the mouth.
But if you’ve gone to see your Dentist and had some procedures performed, how do you know when to be concerned about any pain you are feeling, and how do you know when to just pop a Panadol and rest it off?
There are a few factors that affect the answer to this question – the procedures you had performed, the state of your teeth before the procedures, and whether you were in any pain then.
Your Dentist should have had this discussion with you in the clinic, so you knew what to expect afterwards.
But perhaps you were feeling too light-headed, too drowsy, maybe it was too much information to take in, or you were just in too much pain to listen!
Today I’ll discuss with you the what to expect after a Dental visit – the levels of pain you might feel, how to treat it, and when you should give your Dentist a call for some guidance.
When is Pain “Normal”?
This really is all on a case by case basis – it depends on the procedure, and the person.
However, I’ll give you some advice on what to expect, so you can know what level of pain is normal for your procedure, what is not, and what you should do about it.
If you’ve had any form dental procedure performed at all, expect to feel at least a small amount of discomfort and pain afterwards.
The tenderness you are going to feel may be simply because you’ve received an injection.

Any work performed in the mouth, even a cleaning treatment, is going make you more susceptible to pain.
This is because your mouth is a highly sensitive area – there are more nerves in your mouth than anywhere else in your body, and it’s not used to having someone hold it wide open, and poke around in there with tools!
Your Dentist should give you an aftercare plan following your procedure.
Make sure you follow their instructions, especially if they tell you to take a Panadol – this is your Dentist telling you to expect pain. This is usually after a surgery, extraction, or a root canal therapy .
After these procedures, you are going to need to have painkillers and allow your teeth time to settle down.

Panadol can help for low to mild Dental pain, but it’s always best to consult with your Dentist
If you’ve only had a filling done , it all depends on how deep the filling is. Your Dentist will advise you whether you are going to feel sensitivity, or any forms of pain.
Sometimes a Panadol may be necessary in your case, sometimes it may not – it depends on how deep the filling has gone, especially if it is close to your nerve.
If the filling has gone very close to your nerve, the nerve may become infected, and you may begin to feel excruciating pain.
Any cases of excruciating pain, or even anything that you are slightly unsure of, should be followed up by calling your Dentist and asking for advice.
Any mild sense of pain that you feel, anything can be classified as “normal”, can be treated yourself at home by taking a Panadol or Nurofen. An ice pack on the area that is hurting can also help.
However, if you begin to feel anything you think is out of the ordinary (look out for the symptoms listed below), call your Dentist and they will give you guidance, having known the procedure you had performed.
10 Symptoms you Should be Concerned about
Your Dentist should give you an aftercare plan, to help you avoid getting any possible complications from your procedure.
It’s very important that you follow every step of this plan.
If you happen to notice any of the following, you should also contact your Dentist immediately for their guidance.
#1 Excruciating or throbbing pain, bleeding, or swelling
Contact your Dentist to discuss these symptoms immediately, as these are signs of a possible infection or fractured tooth.
This may be a reaction to the local anaesthetics your Dentist used to numb the pain, most likely before performing an extraction or fixing dentures. It’s normal for the feeling of nausea to last up to 5 days.
If you’re still feeling unwell after 5 days, it’s time to call your Dentist – you may even find that the back part of your dentures requires reshaping.
#3 Earaches or other Facial Pain
Having your mouth open during a dental treatment can cause earaches, leave you hearing that hideous ringing noise, or even like your ear is clogged and you can’t get it clean.

If you experience an earache after a Dental visit, best practice is to contact your Dentist ASAP.
The pain may also affect your eye or other areas of your face.
By this stage, you will probably be having trouble sleeping. These can be signs of an infection, or that your teeth are misaligned.
Speak to your Dentist ASAP to find your answer as to why?
#4 Experiencing Pressure
A white (composite) filling may cause you more irritation than a silver (amalgam) filling.
The dental glue and UV treatment that is used when placing and hardening the white fillings on your teeth makes the composite material shrink, causing a feeling of pressure. This can lead to tooth sensitivity when you bite.
Within a few weeks this issue should have resolved itself, but if you’re still feeling high levels of discomfort, especially pressure and throbbing, contact your Dentist.
#5 Increasing Levels of Pain
Your pain should decrease over the days following surgery.
If you find the pain suddenly increasing after several days, you may have what is known as a “dry socket” and must contact your Dentist immediately.

Dry socket is bone pain that occurs when you have lost the protective blood clot that should have formed after tooth extraction – it has dissolved or dislodged itself from your tooth.
As such, your wound has not had time to heal properly, and your underlying bone and nerves are left exposed to air, foods, and liquids, all of which can cause excruciating pain.
You may also get bad breath or an unpleasant taste in your mouth, a headache or a fever. Your Dentist may use a simple paste to relieve your pain and protect the exposed area, allowing it to heal, or you may need a dressing on the extraction site.
You may also need antibiotics and painkillers to help you through the pain. Always speak to your Dentist or Doctor first.
#6 Jaw Muscle Fatigue
A very common reason for being in pain after visiting your Dentist is from keeping your mouth widen open for so long. It can result in a sore jaw, stiffness, and tired, shaking muscles.
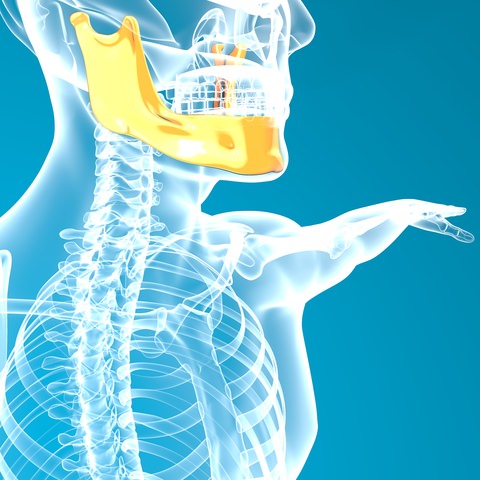
You may experience pain in and around your Jawbone. If it increases, best to speak to your Dentist
A slightly sore jaw is normal after any dental procedure, and that’s when you pop a Panadol and sleep it off.
For longer procedures, like root canals, this pain may last several days.
However, if the pain is severe – for example, if the Panadol isn’t doing anything to help relieve you – contact your Dentist. They will probably recommend an ice pack and give you exercises to relieve the pain.
If you feel as though your jaw is locked in place, that you cannot open and close your mouth easily, you may have “trismus” (sometimes called lockjaw).
Trismus is a spasm of your jaw muscles that causes your mouth to remain tightly shut. It may occur as a result of an injection, especially on your lower teeth, or from jaw strain (from keeping your mouth open for such an extended period).
Generally, trismus lasts from 2 – 3 weeks, but I recommended you contact your Dentist for advice – they will probably offer you the same treatments as muscle fatigue but may also recommend changes to your diet and muscle relaxants if your case is serious.
#8 Sore Throat
Also caused by having your mouth open for so long during your procedure, dehydration can cause a sore throat.
Try drinking lots of water afterwards, or even coconut water, and avoid flavoured water and soft drinks.

If you experience a sore throat, try drinking water to hydrate yourself.
If this doesn’t help, and your throat is severely sore after a few days, you may have an infection, or be having a reaction to the local anaesthetic. Once again, contact your Dentist for guidance.
#9 Soft Tissue Pain
There is a chance you can cause trauma to your tongue during or after a dental procedure, leading to soft tissue pain.
This is why it is very important to listen to your Dentist about when and what you can eat after your treatment if you have had a lot of anaesthetic – eating food that requires a lot of chewing tends to be discouraged as there is a high chance you could bite your tongue, as is avoiding hot drinks as you may burn your tongue.
There is also a possibility you may have accidentally bit your tongue during your procedure.
If you begin to feel any throbbing pain, sensitivity when chewing food, and sensitivity to hot temperatures, contact your Dentist as there is a chance you could have an infection, which they will treat with an antibiotic.
#10 Swelling
Slight swelling immediately after your dental procedure is normal – your body will send extra blood to the injured area to help speed up the healing process.
Using an icepack for 2 days after treatment will help reduce swelling.
However, if it does not get better, or continuously gets worse after 3 days, contact your Dentist – there is a high chance you may have an infection.
Remember – “normal” is that there is always going to be at least a slight amount of pain after any dental procedure.
Try to avoid any complications by ensuring that you stick to your aftercare routine set by your Dentist, and gong to your regular check-ups and maintenance – this is all restorative care for your teeth!
Whatever you do, don’t avoid the Dentist because you’re scared of the pain – the longer you stay away, the more likely it is that you are going to need more painful and expensive treatments in the future!
Is the fear of the dentist that is keeping you away? See our article “How to Reduce Panic Attacks at the Dentist”, and fear no more!

By Dr Veronica Roller
Created at October 11, 2019, Updated at March 06, 2020
No Comments
Leave a comment cancel reply, related posts.

7 Tools All Dentists Use & How They are Cleaned

Mouth Tape – The Ultimate Review!

Dental Records – What Happens When You Die?
12617 Louetta Rd Suite #204 Cypress, TX 77429
[email protected], (281) 376-4444, office hours.

<script src="https://2e353ed9a13e444091b616941cf64484.js.ubembed.com" async></script>
Managing Jaw Pain After Dental Work: A Dentist’s Guide to Opioid Alternatives

The challenges of both acute and chronic pain management have certainly caught the attention of healthcare providers across the country as the opioid pandemic has demanded more responsible prescribing practices. As training and awareness in the prescription of opioids leads to new frameworks for the management of pain, prescribers have become increasingly reliant on non-narcotic strategies.
Dental procedures—and particularly dental surgery—typically require both pre-procedural and post-procedural pain protocols, and in the past, dentists have been lenient and generous with the prescription pad. Unfortunately, it has resulted in the same addictive outcomes seen in the healthcare industry at large, and practices are increasingly facing the need to approach pain with a priority on safety. Complete freedom from pain through over-prescribing of opioids is no longer a viable solution, and dentists must instead focus on creating responsible and effective plans to manage pain appropriately.
Common Types of Jaw Pain
While most dental procedures come with at least a little mild discomfort, some result in considerable pain that requires ongoing treatment. Surgeries and complications can cause inflammation, incisions and extractions need time to heal, patients experience muscle fatigue, and there are a host of possible post-surgical issues.
Here are some common dental issues that may require significant medication protocols to manage pain.
Necrotic Tooth
All teeth have nerves underneath the outer layers of enamel and dentin. Occasionally, due to a deep cavity or extreme biting force, a tooth nerve will die, leaving necrotic tissue inside the tooth. As the body recognizes the infected issue, it builds up an immune reaction which is typically referred to as a tooth abscess. Antibiotics can help alleviate the symptoms of pain and swelling, but only a root canal procedure or a dental extraction will completely resolve a necrotic tooth.
Pulpitis is an inflammation of the pulp of the tooth that can cause severe pain when exposed to things like hot or cold. There are two types of pulpitis: reversible and irreversible. Reversible pulpitis is characterized by pain that resolves when the stimulus is removed, and irreversible pulpitis results in discomfort that is constant and ongoing.
On occasion, pulpitis can be caused by the preparation or drilling of a tooth during the dental procedure itself. If it doesn’t subside within a couple of days following the procedure, another visit to the dentist is warranted as well as further pain management considerations.
Temporomandibular Disorder (TMD)
Frequently referred to as TMJ, temporomandibular disorder refers to pain emanating from the masticatory system. This includes the temporomandibular joint, the muscles of mastication, and the teeth.
TMD can often be misdiagnosed, as it can cause diffuse jaw pain, ear pain, and tooth pain that is difficult to localize. Dentists are well equipped to differentiate TMD pain vs. other types of oral pain, and can mitigate the symptoms with a variety of treatments including specialized mouth pieces, orthodontics, and tooth adjustment. Physical therapy and chiropractic treatment have also proven to be good methods to treat patients suffering from temporomandibular disorder.
Dry sockets can occur following a tooth extraction when the blood clot in the empty socket is disrupted. A dry socket is bone irritation, and can cause deep and intense jaw pain after dental work radiating from the site of the extraction down the side of the face.
Because dry sockets are caused by the disruption of a protective clot, patients should be instructed to avoid any sucking motions that irritate the site. Dentists may decide to use dry socket paste to alleviate the bone pain before medication is prescribed.
Past Approaches to Post-Procedural Pain
Past approaches to managing pain were often driven by the consideration of pain as the 5th vital sign. This resulted in prescribing practices that were designed to largely alleviate or eliminate a patient’s experience of pain.
Unfortunately, while opioids are extremely effective pain remedies, their addictive properties made relatively simple dental procedures a potential entry point for long-term addiction. Little consideration about reasonable pain expectations and root causes—in addition to limited counseling on proper opioid usage—created a perfect storm of routine dental prescriptions and the enablement of patient addiction.

Current Best Practices
Today, responsible management of dental pain means having a larger conversation with patients about reasonable post-procedural expectations, alternative management strategies, and deliberate, informed use of pain medication. Jaw pain after dental work is an inflammatory process, and it’s reasonable for patients to experience some degree of discomfort after a procedure.
Preparing a patient begins with coaching them about the procedure and what kinds of pain to expect. Advice about at-home strategies for pain management like avoiding hot or cold foods and drinks, application of ice packs, and which activities to limit all empower patients to become active participants in their own comfort. Supporting non-opioid pain protocols like steroids for inflammation and medications like acetaminophen and ibuprofen are often enough to reduce pain to tolerable levels. A lot of this can be handled over the phone without the need for pharmaceutical oversight, and should additional medication become necessary, there are a variety of suitable opioid alternatives to consider.
Finally, clear guidelines for follow ups can be extremely helpful for patient decision making. Simply knowing the difference between common and concerning symptoms can be enough to avoid unnecessary office visits, and guidance for adjusting doses on non-opioid pain medications can mitigate temporary increases in discomfort.
Keep Your Practice Current with Premiere
Managing jaw pain after dental work sometimes requires powerful pills, but in modern practice there are a host of non-opioid alternatives and strategies that are improving overall health outcomes. However, because dental practices are often privately owned and operated, disseminating information, establishing industry-wide best practices, and accessing continuing education remain significant challenges for the more than 200,000 dentists currently working in the U.S. today.
Premiere is placing itself at the forefront of dental continuing education, offering an interprofessional perspective on complex healthcare challenges that involve a wide range of health disciplines. Our expert online content is making it easy for dental professionals to stay compliant, informed, and up to date on the latest best practices and industry insights.
Course like This is Such a Pain in the…Mouth! How to Treat Oral Pain and the Role of Opioids developed by Grant Hunsicker, DDS, General Dentist, Hunsicker Family Dental, and Megan Arbour, PhD, RN, CNM, CNE, Associate Professor, Frontier Nursing University deliver key content for dental license renewal requirements that will ensure you give your patients the best possible care. All content by Premiere is created by leading industry professionals, and makes advancing your career and practice as easy as the click of a button.

Related Posts

Vulnerability and Criteria for Alcohol Use Disorder

An Interview with Briana Bloembergen: Examining the Role of the Nurse-Midwife and the Benefits of Physiologic Birth

The Psychological Effects of Losing a Child: How to Manage Trauma as a Healthcare Professional
Your session is about to expire..
You will be timed out in next 4:59 minutes due to inactivity. Please choose to stay signed in or log off.
Do you want to continue your session?

- The Team at Carolina TMJ
- TMJ & Facial Pain Provider
- Testimonials
- Privacy Policy
- Braces for TMJ
- Ultrasound Therapy
- Lower Level Laser Therapy
- Headaches & Trigger Points
- Sleep Disorders
- TMJ & Headache Referral Form
- Snoring & Mild to Moderate Obstructive Sleep Apnea Referral Form
Why Does My Jaw Hurt After a Dental Procedure?
Home » Blog » Why Does My Jaw Hurt After a Dental Procedure?
This is a very common question that we get at Carolina TMJ. Sometimes new patients come in with no jaw pain or limitation in opening before a dental procedure or extraction, begin experiencing pain or limitation after a procedure. While you may think this is because your dentist did something wrong, the vast majority of the time, that’s not the case.
Reasons For Jaw Pain
Typically, jaw pain after a dental procedure is the result of a chronic or underlying jaw condition. Here are the most common reasons for jaw pain and how we diagnose these conditions:
- Trismus
This is the involuntary contraction of the jaw muscles, sometimes due to inflammation of those muscles. This inflammation will contribute to muscle irritation and spasm. Trismus is typically treated with muscle relaxers, NSAIDs, and jaw stretches. When this becomes chronic in nature, or the above treatments do not seem to do the trick, patients come to see me for relief.
- Temporal Tendonitis
Temporal tendonitis is the inflammation of the temporal tendon which connects the temporal muscle on the side of the head to the mandible. Symptoms of temporal tendonitis can include:
- Limitation in opening the mouth
- Pain/pressure behind the eye
- Temporal head pain that can radiate to the forehead
- Ear pain/congestion
- Pain/swelling in the cheek
- Teeth sensitivity
Occlusal wear (loss of tooth structure) on a patient’s teeth, possible arthritis occurring in a patient’s joint, or a history of clenching can all contribute to temporal tendon inflammation. This condition is harder to treat through medication alone, and we have several ways that we treat this condition successfully in our practice every day. Proper diagnosing is crucial as a first step, as it allows us to create a more effective treatment plan.
- Arthritic Joint
It is possible that you had an arthritic process already occurring in one or both of your temporomandibular joints, and the dental procedure aggravated both your joint and the soft tissue supporting your joint. Your temporomandibular joint is used more than any other joint in your body, and it can develop the same issues as your other joints, including arthritis.
We have a protocol we follow for most of our patients with arthritic joints. It can involve custom orthotic therapy, injection therapy, and/or medication, and there are instances that we will refer a patient for further x-rays or MRI.
- Closed Locked
Although it is a rare occurrence, it is true that a patient can become locked after a dental procedure. The reason this happens is based upon how the patient’s joint relates to the articular disc prior to the dental appointment. Here is the ideal joint/disc relationship and a view of the anterior displaced disc/joint:
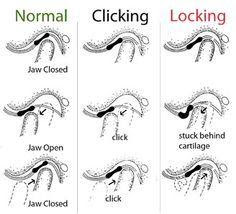
Many patients come in with a disc anteriorly positioned to the joint without actual joint pain. These are patients that have clicks or pops when opening/closing, chewing, etc, but have no pain with the click. It is usually inflammation or a change in the shape of the disc that causes a patient to lock closed (the joint not able to reduce or click onto the disc).
When this occurs, pain will follow along with a limitation of opening and movement of the jaw. Often these patients share that their jaw clicked prior to the dental procedure, but now no longer clicks and they are now very limited in opening and have moderate to severe discomfort when attempting to open.
Let Dr. Davidian Relieve Your Jaw Pain
As you can see, there are many reasons why your jaw may now feel discomfort after a dental procedure or extraction. If you have attempted to resolve this discomfort and have been unsuccessful, you are not alone. We’re here to help you find relief. You can contact our office and schedule your appointment by calling us at 919-782-9955 or requesting an appointment online . We look forward to meeting you and helping you become pain free.
No comment Add yours.
Add your comment cancel reply.
Your email address will not be published.

Pain After Visiting Dentist – Why is it Sore or Numb?
Dental procedures are critical to maintaining oral health, but sometimes they can leave you with soreness or numbness in your mouth. Let’s explain why pain or numbness may occur after a dental visit and how to manage and alleviate these symptoms.
Understanding the Types of Dental Pain
After a dental procedure, it is common for patients to experience some degree of discomfort, soreness, or numbness. The intensity and duration of these sensations can vary depending on the type of procedure performed, individual pain thresholds, and other factors. Understanding why these sensations occur and knowing how to deal with them can ease concerns and aid recovery.
1. Soreness
- Gum and Tooth Soreness : After procedures like dental cleanings, fillings , extractions, or the placement of crowns and braces, the teeth and gums may feel sore. This is often due to the manipulation of teeth and surrounding tissues during the procedure.
- Jaw Soreness : Holding the mouth open for extended periods during a dental procedure can strain the jaw muscles, leading to soreness and discomfort in the jaw.
2. Numbness Dental procedures often require local anesthesia to numb the area being worked on. This can leave the patient with a numb sensation in the mouth, lips, tongue, or even part of the face for several hours after the procedure.
Reasons for Pain or Numbness After a Dental Visit
- Anesthesia : Numbness after dental procedures is usually due to the local anesthesia used to prevent pain during the treatment. The numbness can last for several hours but is temporary.
- Irritation of Oral Tissues : During dental procedures, the mouth is kept open, and instruments are used in the oral cavity. This can cause irritation to the gums, cheeks, and tongue, resulting in soreness.
- Tooth Sensitivity : After a dental cleaning or restoration, teeth may become temporarily more sensitive to temperature changes or pressure.
- Post-Operative Inflammation : After surgical procedures like tooth extractions, the body’s natural inflammatory response can cause swelling and pain in the affected area.
Managing Pain and Numbness
- Cold Compress : Applying a cold compress to the sore area outside the mouth can reduce inflammation and alleviate pain.
- Pain Relievers : Over-the-counter pain relievers such as ibuprofen or acetaminophen can be taken to manage discomfort. Consult your dentist for the recommended dosage.
- Rinse with Warm Saltwater : Rinsing the mouth with warm saltwater can soothe sore oral tissues. Do this gently to avoid dislodging any blood clots after surgical procedures.
- Avoiding Certain Foods and Beverages : Stay away from hot or cold foods and drinks if your teeth are sensitive. Also, avoid chewing on the side of the mouth that is sore or numb.
- Be Cautious with Numb Areas : While your mouth is numb, be careful not to bite your cheeks, lips, or tongue. Also, avoid eating hard or hot foods that could cause burns or injuries that you may not feel while the area is numb.
When to Contact Your Dentist
While mild pain and numbness are normal, if you experience severe pain, swelling, or signs of infection such as fever, or if the numbness lasts for an unusually long time, it’s important to contact your dentist.
Bottom Line Pain, soreness, or numbness after a dental visit is usually a normal part of the healing process. However, proper care and monitoring of these symptoms are essential for a smooth recovery. Patients should follow the dentist’s post-operative instructions closely and not hesitate to reach out to their dentist if they have concerns about the pain or numbness experienced.

You May Also Like

Sensitive Teeth: Toothpaste, Home Remedy, After Filling Crown, Whitening, Pregnancy, to Cold
Can you feel craze lines with your tongue, oral leukoplakia (ol) – treatment, causes, images, tongue, differential diagnosis, leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

Canker Sore After Dentist Visit: Why & How To Treat Properly!
Canker sores after dental treatment
Which dental work causes mouth sores.
Aphthous ulcers, also known as canker sores, are a common oral health problem. They appear as round, yellowish or whitish ulcers on the mouth’s lips, cheeks, tongue, and floor. They are often painful and can be single or multiple. Although they are not dangerous and do not cause a fever, they can irritate and make you uncomfortable. If your child develops aphthous ulcers, there is no need to worry – is it possible that you can get one after visiting a dentist?
Canker sores are a common problem that can occur after dental treatment. They are small, painful ulcers that can make it difficult to eat or speak. While there is no cure for canker sores , there are steps that you can take to help reduce their severity and shorten the duration of the outbreak.
If you experience canker sores after dental treatment, here are a few things that you can do to help relieve the pain and speed healing:
- Apply ice or a cold pack to the sore for 10-15 minutes daily. This will help reduce inflammation and pain.
- Take over-the-counter pain medications such as ibuprofen or acetaminophen to help relieve pain.
- Rinse your mouth with salt water several times a day to help keep the area clean and help promote healing.
- Avoid eating acidic or spicy foods, as these can aggravate the sore and prolong the healing process.
- If necessary, you may also want to consider taking an over-the-counter oral steroid medication to help reduce inflammation and speed healing.
If you experience canker sores after dental treatment, there are a few things that you can do to help reduce their severity and shorten the duration of the outbreak. Following these tips can help keep your mouth healthy and pain-free.
Is it common to get a canker sore after dental work?
Canker sores are a common problem that can occur after dental treatment. They are small, painful ulcers that can make it difficult to eat or speak. While there is no cure for canker sores, there are steps that you can take to help reduce their severity and shorten the duration of the outbreak.

Any dental work can potentially cause canker sores.
Common triggers include:
- tooth extractions
- dental cleaning
- dental injection (novocaine shot)
- wisdom tooth removal
If you have a canker sore, you may notice a tingling or burning sensation a day or two before the sore appears. The sore is usually round or oval and white or yellow with a red border. Canker sores typically heal within two to three weeks without treatment. However, they can be painful and make it difficult to eat or drink.

How To Fix Receding Gums At Home & Other Possible Treatments!

Should You Floss Teeth Twice A Day? Can You Floss Too Much?

Stabilizing Smiles: A Comprehensive Guide to Treating Loose Teeth

Navigating Dental Accidents: A Comprehensive Guide to Prevention, Emergency Response, and Recovery

Mouth Sores from Chemo: Causes, Prevention, and Treatment

What Does a Canker Sore Look Like? Identifying Symptoms and Treatment Options
Privacy Policy
- Orthodontics Niche Guest Post Offer: Write for Us and Share Your Expertise
- Write for Us in the Dentistry Niche: Guest Post Offer

Compare items
- Total ( 0 )

Nelsons Books
Health Resources and More

Jaw Pain After Dental Cleaning: What Do You Need To Know?
Millions of people get their teeth professionally cleaned every year, and jaw pain after dental cleaning is somewhat uncommon to experience. However, there are different types of jaw pain reported after getting dental treatment . This condition can imply an underlying cause due to a mistake performed by your dentist. If you have had previous dental work and you still experience some discomfort, perhaps you need to go to a dental clinic to alleviate the pain .
About Jaw pain After Dental Procedure
A few individuals discover that they encounter pain in their jaw after they got dental treatment. A significant number of the most typical dental jaw issues are reported after an appointment with the dentist .
At times, if you encounter dental jaw pain, it may be because your dentist has committed an error or been careless in your care. If so, and you are, as a result, you might be qualified to make a case for dental negligence compensation.
Types Of Jaw Pain After Dental Work
Jaw pain after dental injection.
It is normal to experience some tenderness or pain after a dental procedure that needed an anesthetic injection. Sometimes, this procedure can feel like the pain is transmitting from your jaw. Mostly, this uneasiness will not keep going for more than a couple of days at most and should disappear all alone. Nevertheless, suppose jaw swelling and pain after dental anesthesia goes on for more than this or begins deteriorating. In that case, it could be an indication of infection. This could also be a sign that you have been harmed while going through the method.
Jaw Pain After Root Canal Treatment
Tooth sensitivity after root canal treatment is common happen. Sometimes, you can feel the pain in your gums and jaw and should vanish on its own. However, if tooth sensitivity persists longer than a few days, the treatment may have caused complication
There are many possible reasons for tooth sensitivity and jaw pain after root canal treatment. Most of the time, tooth sensitivity happens because of an infection or a large filling. Jaw swelling and soreness might occur because the patient’s mouth remains open for a prolonged period. This can cause tension in the jaw muscles, resulting in soreness and pain.
Stiff Jaw After Multiple Dental Procedures
The most usual form of jaw discomfort after dental procedures is the point at which your jaw feels stiff and throbs after you have gone through dental work. Usually, similar to root canal treatment above, this kind of jaw pain originates from your mouth because of being open for an extended time. This can cause strain on your jaw muscles, resulting in jaw swelling and pain. The agony should disappear all alone within a couple of days if you simply have a stressed jaw muscle after getting one or two dental procedures. Nonetheless, suppose the discomfort does not disappear all alone or begins to deteriorate. In that case, it could be an indication of something more serious. You must visit your dentist if this is the condition to know if you require any further dental procedures to address the issue.
Jaw Pain After Dental Cleaning
Some individuals encounter jaw pain after dental cleaning. This is rare to happen, but it is possible that dental cleaning can cause jaw swelling and pain, particularly with those temporomandibular joint problems (TMJ).
Jaw pain after dental cleaning is typically simply due to the strain and tension of having your mouth open in a strange situation for a prolonged period. Nevertheless, suppose jaw pain after deep dental cleaning does not fade all alone after a couple of days, or if it deteriorates. In that case, it could be a sign that something else is not correct. You should revisit your dentist to check whether you need any other dental treatment.
Jaw Pain After Dental Implant
As this technique includes drilling your jawbone, it is usual to have some pain in the days after the procedure as you begin to mend. In any case, if you have jaw swelling and pain for more than this, or if it starts to get worse, it could be a sign of something being off-base.
After implant surgery, reasons for jaw pain could demonstrate an infection at the area of the implant or trauma to the encompassing region or another tooth. This kind of problem does not necessarily imply that your dentist committed mistakes. However, at times, dental carelessness can mean that you are avoidably harmed during the method, which can prompt further issues.
Dental Abscess Jaw Pain
Suppose you encounter pain in your jaw after dental treatment, which is persistent and pounding in nature. In that case, it could imply that you are fostering an abscess. Basically, a dental abscess is a kind of bacterial disease that makes pus collect in the space of your mouth and can be joined by jaw swelling. This is a pain that disseminates to your ear or neck just as the influenced area of the jaw, unpleasant taste in your mouth, and tooth sensitivity to hot or cold drinks or food.
If the infection will not address rapidly, it can likewise cause you to feel very unwell. With a high temperature, the pain and swelling can cause some trouble with swallowing or even breathing.
A dental abscess causing jaw pain does not generally imply that your dentist was negligent when they treated you. However, if they conveyed care that was not up to standard and you have suffered. As a result, you may be qualified to make a case for dental carelessness compensation.
You can contact Oakleigh Smiles today if you need a professional to assess your situation.
References:
Temporomandibular Disorder (TMD).
https://www.hopkinsmedicine.org/health/conditions-and-diseases/temporomandibular-disorder-tmd
What’s to know about dental abscesses?
https://www.medicalnewstoday.com/articles/170136

Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Recent Post
- Jaw Pain After Dental Work Can’t Open Mouth: Understanding and Managing Post-Procedure Discomfort March 13, 2024
- How to Relieve Tooth Pain After Filling: Discover Effective Methods February 12, 2024
- Jaw Sore After Filling: Causes, Remedies, and Prevention January 15, 2024
- Jaw Pain After Tooth Extraction: What You Need to Know December 12, 2023
- Underbite Jaw Surgery: Procedure Benefits and Risks November 13, 2023
- Aesthetics (1)
- Dental Care (19)
- Dental Health (15)
- Health Tips (65)
- Medical (9)
- Oral Care (4)
- Tooth Care (22)
- Uncategorized (15)

IMAGES
VIDEO
COMMENTS
Most people will see their jaw or TMJ discomfort gradually improve in the days after their dental procedure. However, if symptoms persist for more than two weeks, it's important to see your dentist or oral surgeon for a consultation. Your dentist may prescribe a muscle relaxer to help jump-start your recovery from a sore jaw.
1. Jaw Muscle Fatigue. What it is: Jaw muscle pain after dental work, like a filling or root canal, is muscle soreness caused by having the mouth open for a long time.People that grind their teeth a lot are more susceptible to this condition because their temporomandibular joint is already strained.. What it feels like: The jaw muscles give out, much like your leg muscles when running until ...
Long-Term Pain Management and Prevention. For persistent jaw pain resulting from dental work or underlying conditions like TMJ disorder, my approach often involves a combination of physical therapy, jaw exercises, and possibly a nightguard or bite splint to prevent stress from teeth grinding.Anti-inflammatory medications and muscle relaxants can be used to manage muscle spasms.
It also depends on the actual cause of the TMJ pain after you got dental work done. If it was caused by the dental injection, the pain and discomfort will likely go away in just two or three days. If you're lucky, your jaw might even start feeling comfortable again just hours after your procedure. But if the jaw pain is a result of keeping ...
Jaw and muscle strain/sprain, sometimes called JAMSS, is a localized acute musculoskeletal disorder that can result from a traumatic or mechanical injury. It can cause sudden jaw pain, limited range of motion, tenderness, or dysfunction. Trauma to the jaw includes a direct blow, previous injuries, bruxism (clenching/grinding), yawning too wide ...
Jaw pain is a common issue that affects millions of people in the U.S. Jaw pain may be mild or can be severe and affect your quality of life. Many factors can cause jaw pain, such as grinding your teeth, gum disease or a toothache. Jaw pain may also be a symptom of a serious issue, including a broken or dislocated jaw or a heart attack.
Acute jaw joint and muscle sprain/strain after dental procedures is more common than originally thought with more than 50% of patients with temporomandibular disorders (TMD) reporting their pain onset as a direct result of dental care.1-13 In one study of 164 patients with TMD, trauma was the initiating factor in 50.6% of cases, with 61% of ...
Swelling and pain. Swelling is common after certain dental procedures, particularly tooth removal (extraction) and periodontal surgery. Holding an ice pack—or better yet, a plastic bag of frozen peas or corn (which adapts to the shape of the face)—to the cheek can prevent much of the swelling. Ice therapy can be used for the first 18 hours.
Jaw Pain After Dental Work. Any dental procedure that requires you to keep your mouth open for an extended period can result in soreness and stiffness due to muscle strain. A slightly sore jaw is normal following dental treatment, but if the pain is severe, call your dentist. They may suggest warm, moist compresses and gentle stretching exercises.
Here's how it works: Persistent muscle tension after a strain injury leads to decreased oxygenation, muscle fatigue, and more pain. Soon, routine use of the jaw during eating or mouth opening begins to trigger pain signals. When these pain signals are persistent, they induce a hyperexcitable state in the neurons of the central nervous system.
Some of the most common TMJ symptoms you may experience after dental work include: Pain and/or pressure in the jaw, face, ears, or neck. Jaw stiffness. Jaw popping and clicking. Difficulties opening and closing the jaw. Locking of the jaw joints. Headaches.
Try this: Put your tongue on the roof of your mouth. Open your mouth as far as possible with your tongue remaining in contact with the roof of your mouth. (Maintaining the contact prevents you ...
It can result in a sore jaw, stiffness, and tired, shaking muscles. You may experience pain in and around your Jawbone. If it increases, best to speak to your Dentist. A slightly sore jaw is normal after any dental procedure, and that's when you pop a Panadol and sleep it off. For longer procedures, like root canals, this pain may last ...
· Ibuprofen and other painkillers may also help to minimize your jaw pain after dental work. · If ibuprofen or similar medicine doesn't help, your dentist might prescribe a muscle relaxant to reduce the pain. When to Visit a Dentist For Jaw Pain. Any discomfort or sensitivity you feel after a filling should go away after a few weeks. If ...
Today, responsible management of dental pain means having a larger conversation with patients about reasonable post-procedural expectations, alternative management strategies, and deliberate, informed use of pain medication. Jaw pain after dental work is an inflammatory process, and it's reasonable for patients to experience some degree of ...
After the Visit. If your mouth is sore, you can take over-the-counter pain relievers.. Call the office between routine visits if you have questions, your teeth hurt, or your jaw swells. Issues ...
Typically, jaw pain after a dental procedure is the result of a chronic or underlying jaw condition. Here are the most common reasons for jaw pain and how we diagnose these conditions: Trismus. This is the involuntary contraction of the jaw muscles, sometimes due to inflammation of those muscles. This inflammation will contribute to muscle ...
1. Soreness. Gum and Tooth Soreness: After procedures like dental cleanings, fillings, extractions, or the placement of crowns and braces, the teeth and gums may feel sore. This is often due to the manipulation of teeth and surrounding tissues during the procedure. Jaw Soreness: Holding the mouth open for extended periods during a dental ...
Apply ice or a cold pack to the sore for 10-15 minutes daily. This will help reduce inflammation and pain. Take over-the-counter pain medications such as ibuprofen or acetaminophen to help relieve pain. Rinse your mouth with salt water several times a day to help keep the area clean and help promote healing. Avoid eating acidic or spicy foods ...
TMJ (also referred to as TMD) is a joint disorder that involves the temporomandibular joint. This sliding joint connects the lower jaw with your skull at a point right in front of each ear. Even when the causes of TMJ are managed, a TMJ flare up after dental work is a fairly common occurrence. If this.
Sudden neck and lower jaw pain can signal an emergency. Call 911, especially if you have known heart problems. All other tooth, gum, and jaw pain should trigger a call to your dentist — as soon as possible if you suspect a cracked filling or tooth, gum disease, or an abscess. "Bacteria from the abscess can get into the bloodstream, and can ...
Some individuals encounter jaw pain after dental cleaning. This is rare to happen, but it is possible that dental cleaning can cause jaw swelling and pain, particularly with those temporomandibular joint problems (TMJ). Jaw pain after dental cleaning is typically simply due to the strain and tension of having your mouth open in a strange ...
From a dental perspective, acute jaw joint and muscle sprain and strain (JAMSS), often resulting from dental and orofacial trauma, can lead to chronic orofacial pain, temporomandibular disorders, and headache. ... (J.F.) for an urgent visit with severe jaw pain and limited range of motion 1 day after a mandibular nerve block was used to ...