
Is It OK to Fly With High Blood Pressure?

You can fly with hypertension if you take precautions and travel with support. Flying with high blood pressure increases the risk of serious health concerns such as blood clots, pulmonary embolism, stroke and heart failure, but you can reduce these risks with the right guidance, monitoring and care.
Can You Fly if You Have High Blood Pressure?
You can travel with high blood pressure, but the specific precautions you must take depend on your overall health and hypertension stability. Consulting with your doctor before a flight is crucial because your medical provider can determine if it’s safe for you to fly and what you can do to remain safe.
The best way to travel with high blood pressure on an airplane is to fly with medical support. Taking a private air ambulance or traveling with a medical escort helps you access the care you need while in the air.
How Does Flying Affect Blood Pressure?
Flying with high blood pressure presents potential risks due to how high altitudes affect aircraft cabins. A cabin’s oxygen levels decrease once a plane reaches high altitude, forcing the heart to pump harder to move oxygen throughout the body. This extra labor increases stress and blood pressure. While this increase is typically non-concerning for most people, it can lead to serious health complications for individuals with hypertension.
Why Is It Dangerous to Fly With High Blood Pressure?
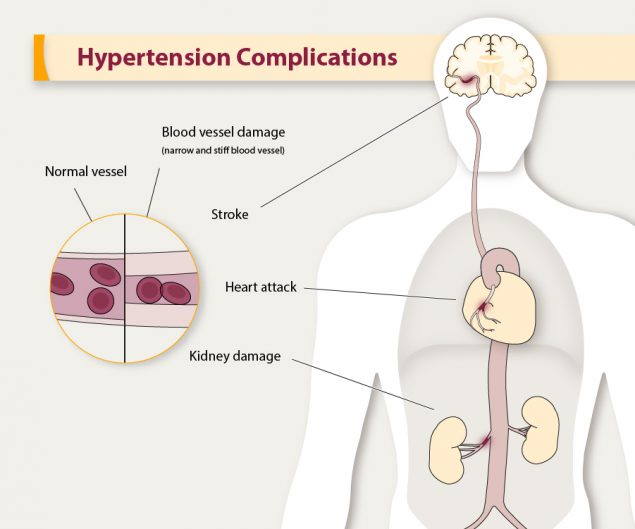
Flying with high blood pressure and no medical support can be dangerous because it presents the following risks:
Significant Spikes in Blood Pressure
Low oxygen levels, salty snacks, and alcoholic beverages can all increase blood pressure. If you have any apprehensions about air travel, anxiety and stress may also increase blood pressure, so it’s important to surround yourself with support.
Deep Vein Thrombosis
Deep vein thrombosis (DVT) involves a blood clot in one of the body’s deep veins. This most commonly occurs in a leg , but it can also develop in the pelvis or an arm. Flying with high blood pressure increases the risk of DVT because sitting for prolonged periods on an aircraft reduces circulation.
DVT requires treatment to prevent the clot from worsening or causing long-term vein complications such as post-thrombotic syndrome (PTS). PTS occurs when a vein’s valves incur damage, which can result in discoloration, pain, swelling, ulcers and scaling in the affected area.
Pulmonary Embolism
If left untreated, DVT can turn into a pulmonary embolism . If part of a blood clot breaks off, it can travel to the lungs and cause a blockage in the lungs. Recovery from a small pulmonary embolism is likely with the right treatment, but it may cause lung damage. A significant clot can be fatal if it stops the lungs from receiving blood.
DVT can also lead to hypoxia, which refers to low oxygen levels in your body’s tissues. Hypoxia can cause the following symptoms and complications:
- Rapid heart rate
- Difficulty breathing
- A bluish tint to the skin
- Restlessness
Increased Risk of Serious Heart Conditions
Since flying can exacerbate high blood pressure, it also increases the risk of serious heart conditions such as stroke and heart failure. A stroke occurs when a blockage prevents the brain from receiving enough blood . It can also occur in the form of a burst blood vessel in the brain, and it can damage portions of the brain.
How to Fly With High Blood Pressure Safely

While hypertension and flying present serious risks, it is OK to fly with high blood pressure as long as you consult with your doctor and take precautions. The following solutions can help you enjoy a safe flight with peace of mind:
1. Fly With Medical Support
Having the right support system during a flight can help you reach your destination safely. Flight attendants receive training for basic life-saving measures such as automated external defibrillators and cardiopulmonary resuscitation, but they cannot provide medical intervention for most serious conditions.
Flying with a trained medical professional can help you remain safe and healthy during your trip, and you can do so in one of the following ways:
- Medical escort: A medical escort is a highly trained individual who can monitor your condition and provide medical intervention if necessary. REVA’s medical escort services provide you with safe, reliable care during your commercial flight so you can fly with peace of mind. A medical escort helps you remain comfortable, watching for signs of potential complications and providing the necessary care if complications arise.
- Air ambulance: An air ambulance flight is ideal for patients who need more intensive care during a flight. When you travel via an air ambulance, an experienced medical and flight team transports you from one location to another on a fully equipped medical aircraft . You may require an air ambulance if you have high blood pressure with additional health concerns.
2. Consume Only Healthy Food and Beverages During Your Flight
Avoiding salty snacks and alcoholic beverages can help you maintain healthy blood pressure on your flight. Before boarding a plane, purchase healthy snacks such as fruit, dried fruit or unsalted nuts. This way, you still have something to eat without consuming the salty options airlines typically offer. It’s also important to opt for water instead of alcohol while flying. Staying hydrated can help you prevent significant blood pressure spikes .
3. Move Around During Your Flight
Movement promotes healthy circulation, which can help prevent DVT. Stand up, stretch and walk around periodically if you can. Getting your blood flowing is especially important during longer flights.
4. Continue Taking Your Blood Pressure Medication as Prescribed
Blood pressure medication is allowed on flights, and taking it as your doctor prescribes it is important. Pack your medication in your carry-on bag so you can easily access it and take it at your regular time.
If you need to take any additional medications, such as motion-sickness pills, talk to your doctor first to ensure they are safe to take with your blood pressure medication.
5. Monitor Your Blood Pressure
Airlines allow passengers to bring blood pressure monitors on board, but they may have restrictions on certain types of batteries. If you fly with a medical escort, they will carry the necessary monitoring devices onto the flight and use them to determine your needs.
Why Trust Us
You can trust REVA with your in-flight medical needs because we prioritize safety above all else. We transport patients on the highest-quality medical aircraft, and our flight and medical teams receive ongoing training to provide the best care possible.
Our medical escorts and medical teams include registered nurses, flight doctors, registered respiratory therapists and critical-care paramedics. Whether you need to travel via an air ambulance or take a medical escort along on a commercial flight, you can count on REVA for safety and peace of mind.
Fly Safely With REVA
You can fly with high blood pressure as long as you take measures to monitor and protect your health during your trip. REVA offers medical escort services and air ambulance flights to transport you safely and comfortably.
Our medical escorts have the training and experience to monitor your blood pressure and overall health, prevent serious health risks and address potential complications if they occur. Contact us to request a quote or learn more about our air ambulance and medical escort services.


NICOLE POWELL-DUNFORD, MD, MPH, JOSEPH R. ADAMS, DO, MPH, AND CHRISTOPHER GRACE, DO, MPH
Am Fam Physician. 2021;104(4):403-410
Related Letter to the Editor: Helping Adults With Dementia Travel by Air
Author disclosure: No relevant financial affiliations.
Air travel is generally safe, but the flight environment poses unique physiologic challenges such as relative hypoxia that may trigger adverse myocardial or pulmonary outcomes. To optimize health outcomes, communication must take place between the traveler, family physician, and airline carrier when there is any doubt about fitness for air travel. Travelers should carry current medications in their original containers and a list of their medical conditions and allergies; they should adjust timing of medications as needed based on time zone changes. The Hypoxia Altitude Simulation Test can be used to determine specific in-flight oxygen requirements for patients who have pulmonary complications or for those for whom safe air travel remains in doubt. Patients with pulmonary conditions who are unable to walk 50 m or for those whose usual oxygen requirements exceed 4 L per minute should be advised not to fly. Trapped gases that expand at high altitude can cause problems for travelers with recent surgery; casting; ear, nose, and throat issues; or dental issues. Insulin requirements may change based on duration and direction of travel. Travelers can minimize risk for deep venous thrombosis by adequately hydrating, avoiding alcohol, walking for 10 to 15 minutes every two hours of travel time, and performing seated isometric exercises. Wearing compression stockings can prevent asymptomatic deep venous thrombosis and superficial venous thrombosis for flights five hours or longer in duration. Physicians and travelers can review relevant pretravel health information, including required and recommended immunizations, health concerns, and other travel resources appropriate for any destination worldwide on the Centers for Disease Control and Prevention travel website.
Air travel has become increasingly popular over time, despite decreases during the COVID-19 pandemic, with 1.1 billion total passengers in 2019 and most Americans having flown at least once in the past three years. 1 Air travel is generally safe, but especially for the aging U.S. population, the flight environment poses unique physiologic challenges, particularly relative hypoxia, which may trigger adverse myocardial or pulmonary outcomes. To optimize health outcomes, communication must take place between the traveler, family physician, and airline carrier when any doubt occurs about fitness for air travel. Travelers should carry current medications in their original containers as well as a list of their medical conditions and allergies and should adjust timing of medications as needed based on time zone changes. Travelers should also consider available medical resources at their travel destinations and layover locations. Family physicians and travelers can review relevant pretravel health information, including required and recommended immunizations, health concerns, and other travel resources appropriate for any destination worldwide at https://wwwnc.cdc.gov/travel/destinations/list .
Pulmonary Conditions
By law, U.S. commercial aircraft cannot exceed a relative cabin altitude of 8,000 feet (2,438 m) because of the potential for significant hypoxia above this altitude. 2 Most passengers exposed to this environment will have a partial pressure of arterial oxygen (Pao 2 ) of 60 to 65 mm Hg (7.98 to 8.64 kPa), corresponding to 89% to 94% peripheral oxygen saturation (Spo 2 ), which may compromise cardiovascular or pulmonary disease in affected travelers. 3 Neither reassuring pulse oximetry nor reassuring forced expiratory volume in one second has been found to predict hypoxemia or in-flight events for patients with pulmonary conditions. 3
The nonstandardized Hypoxia Altitude Simulation Test, administered and interpreted by pulmonologists, can be used to determine specific in-flight oxygen requirements for patients with pulmonary complications or those for whom safe air travel remains in doubt. Typically, the Hypoxia Altitude Simulation Test comprises breathing 15% fraction of inspired oxygen for 20 minutes, with pulse oximeter and blood gas measurements taken before and after testing. 4 – 6 Patients with a Hypoxia Altitude Simulation Test Pao 2 less than 50 mm Hg (6.65 kPa) at any point during the test require supplemental oxygen in flight, whereas those with a Pao 2 greater than 55 mm Hg (7.32 kPa) do not. Pao 2 measurements falling between 50 and 55 mm Hg are considered borderline and may necessitate further testing with activity. 5 Given that the test itself incurs some risk and may not be available to all travelers, family physicians can counsel patients who are unable to walk 50 m (164 ft) or those whose usual oxygen requirements exceed 4 L per minute not to fly. 3 , 4 , 7 , 8
Patients with oxygen requirements less than 4 L per minute can be counseled to double their usual flow rate while flying. 8
Commercial airline carriers usually permit the use of personal Federal Aviation Administration–approved portable oxygen compressors, but carriers require travelers to give from 48 hours to one month's notice before flight when they are requesting the use of compressed oxygen. 9
Table 1 lists indications for which further assessment (e.g., Hypoxia Altitude Simulation Test, ability to walk 50 m) is warranted, including previous respiratory difficulties while flying, severe lung disease, recent or active lung infections, any preexisting oxygen requirements or ventilatory support, or if less than six weeks have passed since hospital discharge for acute respiratory illness. 3 Patients who have undergone an open-chest lung procedure should defer travel for two to three weeks, must not have any recent or residual pneumothorax, and should be assessed for supplemental oxygen needs. 10
Cardiac Conditions
Travelers with underlying cardiac conditions should use airport assistance services such as wheelchairs and baggage trolleys to decrease myocardial oxygen demand. 9 Although most cardiac conditions are safe for flight, some require additional consideration. Travelers with minimally symptomatic, stable heart failure may safely fly, but medication adherence is critical. 9 , 11 Patients with stable angina should be assessed for oxygen needs if they become short of breath after walking 50 m , and they should not fly following any recent medication changes that have not demonstrated clinical stability beyond that medication's half-life. 7 , 11
Patients with unstable angina, new cardiac or pulmonary symptoms, or recent changes in medication without appropriate follow-up should not fly until stable, particularly for medication changes that could impact blood pressure or coronary reserve. 11 Travelers with recent myocardial infarction at low risk should defer air travel for three to 10 days postevent 11 – 15 ( Table 2 11 ) . Low-risk patients who required percutaneous transluminal coronary angioplasty may fly after three days as long as they are asymptomatic. 9 Travelers who have had coronary artery bypass grafting or an uncomplicated open-chest procedure should wait to fly until they are 10 days postprocedure. 7 , 11
Many implantable-cardioverter defibrillators are compatible with standard airport security. 9 The Transportation Security Administration recommends that travelers with pacemakers, defibrillators, or any other implanted metal device request pat-down screening instead of using a walk-through metal detector. 16 For travelers with pacemakers and implantable-cardioverter defibrillators, a two-day flight restriction following uncomplicated placement is appropriate. 11 It is prudent for all cardiac patients to travel with a copy of their most recent electrocardiography results and a preflight graded exercise test, which may aid in assessment and management in case of an event during flight. 9 In patients with hypertension, medication compliance is especially important because aircraft noise and other travel-related stress may provoke blood pressure elevations. 17 Travel in patients with moderately controlled hypertension is not a contraindication, but airline travel for those with uncontrolled hypertension requires shared decision-making and clinical judgment.
Ear, Nose, and Throat Conditions
Trapped gases and sinus air-fluid levels can cause significant pain for the patient with ear, nose, and/or throat conditions. Adult patients with symptomatic rhinosinusitis or allergic rhinitis may benefit from oxymetazoline (Afrin) and/or pseudoephedrine to prevent ear blockage during descent. 18 No evidence suggests that antihistamines or decongestants are beneficial in children with sinusitis, 19 and these medications should not be used to hasten an early clearance for flight in any age group. Flight within 36 hours of otitis media resolution is generally safe. 20 Equalizing pressure on descent can also be accomplished in adults with frequent swallowing, chewing gum or food, or by generating pressure against a closed mouth and glottis. In young children and infants, upright bottle feeding or pacifier use can achieve similar effects. 21
Patients who have undergone jaw fracture repair should defer flying for at least one to two weeks, and jaw wiring should be temporarily replaced with elastic bands in case of emesis. 18 Transdermal scopolamine is effective in preventing air sickness , 22 and alternatives such as first-generation antihistamines may also be useful. Patients who elect to take scopolamine should be counseled on adverse effects of drowsiness, blurry vision, dry mouth, or dizziness. 22 Individuals who are prone to air sickness should refrain from alcohol use during flight and in preflight and should eat smaller, lighter meals. 18 The expansion of trapped gas at altitude may cause severe tooth pain in patients with caries beneath fixed restorations. Travelers with hearing aids should bring extra batteries and all accessories and may need to adjust their volume levels to offset background noise.
Diabetes Mellitus
In addition to carrying all medications, travelers with diabetes requiring insulin should request appropriate meals and consider checking blood glucose levels at intervals during longer flights. 23 Bringing snacks or other food can assist those with tenuous diabetes management in the event of layovers or delays. Insulin requirements may change based on the direction of travel and crossing time zones, which may entail lost or gained hours. Even if it is not part of the patient's normal regimen, fast-acting insulin, ideally with a pen device, should be considered for all travelers during flight due to its flexibility and responsiveness. 23 When traveling east, if the day is shortened by two or more hours, it may be necessary to give less insulin on the first day at the destination. When traveling west, if the day is extended by two or more hours, it may be necessary to give more insulin on the first day at the destination. Blood glucose should be checked at least 10 hours after the first-day dose to allow for further adjustments. Travelers can return to their normal insulin regimen on day 2 at their destination. A comprehensive public access resource for medical professionals addressing insulin adjustment for the air traveler is available through the Aerospace Medical Association. 23
Gastrointestinal Conditions
For travelers with recent intra-abdominal procedures, trapped gas expansion could disrupt sutures and cause rebleeding. Travelers should wait until 24 hours have passed and any bloating has resolved following laparoscopic abdominal procedures or colonoscopy. 7 , 10 Travelers should wait one to two weeks after open abdominal surgery. 10 Patients with active gastrointestinal problems, including hematemesis, melena, or obstruction, should not fly. 24
Hematologic Conditions
A baseline anemia may predispose travelers to syncope given the relative hypoxia of the flight environment. Caution should be exercised for travelers with a hemoglobin level below 8.5 g per dL (85 g per L), and some authorities recommend not advising flight for any travelers with levels below 7.5 g per dL (75 g per L). 7 Young, otherwise healthy patients with chronic anemia may be more tolerant of relative hypoxia, especially if their hemoglobin level is greater than 7.5 g per dL. 24 For the traveler with sickle cell anemia, sickling crisis during flight is unlikely 24 ; however, flight should be delayed for 10 days following an acute crisis, and patients with sickle cell anemia who have received a recent transfusion should not fly if hemoglobin levels are less than 7.5 g per dL. 24
Although deep venous thrombosis (DVT) is not caused by the flight environment itself, DVT is a concern for people who sit for extended periods or have risk factors. 25 Incidence of DVT reaches up to 5.4% in high-risk groups flying an average of 12.4 hours. 26 Compression stockings can prevent asymptomatic DVT and superficial venous thrombosis in flights lasting five hours or longer. 27 Table 3 lists recommendations for DVT prophylaxis for travelers who are at low, moderate, and high risk for DVT. 11 The baseline recommendations for each group include staying hydrated, avoiding alcohol to prevent dehydration, walking at least 10 to 15 minutes in each two hours of travel time, and performing isometric exercises while seated. 11 When indicated for high-risk travelers, including those with reduced mobility, low-molecular-weight heparin (e.g., 40 mg of subcutaneous enoxaparin [Lovenox]) on the day of and day after travel is appropriate for anticoagulation. 28
Psychiatric and Intellectual Disability Conditions
Passengers with mental or intellectual disabilities often benefit from a traveling companion because physiologic stresses of flight and the chaotic nature of busy airports may be especially challenging aspects of travel for these groups. 9 Prescription anxiolytics may alleviate travel anxiety, but a test dose is highly encouraged before flight. 9 Service or emotional support animals can be used for a variety of mental health conditions; an article in American Family Physician provides information about considerations for documentation for emotional support animals. 29 See the U.S. Department of Transportation website for current guidelines regarding the use of these animals during air travel. 30
Neurologic Conditions
Passengers predisposed to stress-related headaches and severe migraines should always carry abortive medications. Travelers with uncontrolled vertigo are not good candidates for flight. Patients prone to syncope should remain well-hydrated and be cautioned to avoid alcohol or quickly standing from a seated position. One small study suggests that people who have epilepsy with a history of flight-related seizures and a high baseline seizure frequency are likely to have a seizure after flying. 31 The Aerospace Medical Association recommends that patients with uncontrolled or poorly controlled seizures should not fly. 32 A safe amount of time permitted before flight following a seizure has not been established, but clinical judgment and the presence of a knowledgeable chaperone should factor into any medical recommendation. Although some airline carriers allow patients to fly 72 hours after a stroke, 7 the Aerospace Medical Association recommends waiting one to two weeks. 32
Obstetric Conditions
Background radiation associated with the flight environment does not pose a special hazard for most pregnant air travelers; however, the Federal Aviation Administration recommends informing aircrew or frequent flyers about health risks of radiation exposure. 33 Because a lack of in-flight medical resources may jeopardize safety of the mother and neonate, patients with an uncomplicated singleton pregnancy should generally not fly beyond 36 weeks of estimated gestational age 7 , 24 , 33 , 34 and those with a multiple gestation not beyond 32 weeks . 7 , 34 Body imaging scanners are safe for security screening during pregnancy. 34 , 35 Postpartum travelers are at moderate risk for DVT and should wear compression stockings and perform isometric exercises during flight. 11 Travelers who have undergone an uncomplicated cesarean delivery are generally safe for flight within one to two weeks. 10
Ophthalmologic Conditions
Passengers with severe visual impairment may benefit from having a traveling companion. Xerophthalmia may be exacerbated in the low humidity of the airplane cabin, and lubricating eye drops are advisable. Cataracts and clinically stable glaucoma are not contraindications to flight; however, any retinal detachment interventions should restrict flight for at least two weeks. 36 Open-globe eye surgery should delay air travel for up to six weeks, and travel recommendations should be made in conjunction with an ophthalmologist. 36
Orthopedic Conditions
Because of expansion of trapped air at altitude, all fixed casts should be bivalved. 7 , 37 Some airlines do not permit air casts of any kind, but if they are used, a small amount of air should be released to prevent any limb compression that occurs as a result of trapped gas expansion. Elastic bandages can be added to a bivalved cast and can be loosened as tolerated. The Transportation Security Administration recommends that passengers with prosthetic limbs should avoid metal detector screening and should be screened with alternative measures. 16 Individuals with significantly decreased mobility should consider wheelchairs and the use of travel companions. Passengers with low back pain and other mobility-limiting conditions can request seating near the front to reduce walking; however, business and first-class seating is an additional cost.
Urologic Conditions
Foley catheters and other inflatable balloons are compatible with flight; however, they should be filled with liquid for air travel, given the previously described expansion of trapped gas at altitude.
Special Considerations for Children
Healthy, term neonates should not fly for at least 48 hours after birth but preferably one to two weeks. 21 Infants younger than one year with a history of chronic respiratory problems since birth should be evaluated by a pulmonologist before air travel. 3
Other Air Travel Considerations
Jet lag occurs as a result of desynchronization between an individual's internal circadian rhythm and the external environment's time zone. 38 , 39 Jet lag is worse for eastward rather than westward travel. 40 Measures for prevention include ensuring enough sleep before travel, timing light exposure using sunglasses, avoiding alcohol, and eating at appropriate times after arriving at the destination. Timed melatonin is highly effective at treating jet lag, 41 and prescription hypnotic-sedative medications may also work in controlling sleep loss. 38
Self-contained underwater breathing apparatus (SCUBA) divers should not fly within 12 hours of a dive because of the concern for decompression sickness or life-threatening arterial gas embolism. 42
The airplane cabin does not inherently pose greater risk for infection than any other close contact, but respiratory viral pathogens are the most commonly transmitted infections. 43 Because of the ongoing COVID-19 pandemic, the Centers for Disease Control and Prevention (CDC) recommends delaying travel until the individual is fully vaccinated because traveling increases the chance of getting and spreading COVID-19. For patients not fully vaccinated who must travel, it is important to follow the CDC's recommendations for unvaccinated people. Check for evolving guidelines on the CDC's website. 44
Patients with breast cancer who have had surgery may fly without risking new or worsening lymphadenopathy. 45
A comprehensive discussion of in-flight emergencies is beyond the scope of this article. See the American Family Physician article on in-flight emergencies for more details. 46
This article updates a previous article on this topic by Bettes and McKenas . 37
Data Sources: A PubMed, Cochrane database, Essential Evidence Plus, ACCESSSS, and ECRI search occurred in April and May 2020 and April and May 2021 using search terms aviation medicine, travel medicine, commercial flight, air travel, and fitness to fly. The Aerospace Medical Association's website resource, Medical Considerations for Airline Travel, was searched in its entirety. The Handbook of Aviation and Space Medicine, Fundamentals of Aerospace Medicine, and Aviation and Space Medicine were reviewed for clinically relevant chapters.
The authors acknowledge Rachel Kinsler, USAARL Research Engineer, for her thoughtful review of this manuscript.
The views, opinions, and/or findings contained in this report are those of the authors and should not be construed as an official Department of the Army position, policy, or decision, unless so designated by other official documentation. Citation of trade names in this report does not constitute an official Department of the Army endorsement or approval of the use of such commercial items.
Airlines for America. Air travelers in America: annual survey. Accessed May 1, 2021. https://www.airlines.org/dataset/air-travelers-in-america-annual-survey/#
14 Code of Federal Regulations §25.841—pressurized cabins. Accessed May 1, 2021. https://www.govinfo.gov/app/details/CFR-2012-title14-vol1/CFR-2012-title14-vol1-sec25-841
- Ahmedzai S, Balfour-Lynn IM, Bewick T, et al.; British Thoracic Society Standards of Care Committee. Managing passengers with stable respiratory disease planning air travel. Thorax. 2011;66(suppl 1):i1-i30.
Respiratory disease. In: Green N, Gaydos S, Hutchinson E, et al., eds. Handbook of Aviation and Space Medicine . CRC Press; 2019:329–333.
Dine CJ, Kreider ME. Hypoxia altitude simulation test. Chest. 2008;133(4):1002-1005.
- Matthys H. Fit for high altitude: are hypoxic challenge tests useful? Multidiscip Respir Med. 2011;6(1):38-46.
Bagshaw M. Commercial passenger fitness to fly. In: Gradwell DP, Rainford DJ, eds. Ernsting's Aviation and Space Medicine . 5th ed. CRC Press; 2016:631–640.
Josephs LK, Coker RK, Thomas M; BTS Air Travel Working Group; British Thoracic Society; Managing patients with stable respiratory disease planning air travel. Prim Care Respir J. 2013;22(2):234-238.
Rayman RB, Williams KA. The passenger and the patient inflight. In: DeHart RL, Davis JR, eds. Fundamentals of Aerospace Medicine . 3rd ed. Lippincott Williams & Wilkins; 2002:453–469.
Aerospace Medical Association. Surgical conditions. May 2003. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Surgical-Conditions.pdf
- Smith D, Toff W, Joy M, et al. Fitness to fly for passengers with cardiovascular disease. Heart. 2010;96(suppl 2):ii1-ii16.
- Thomas MD, Hinds R, Walker C, et al. Safety of aeromedical repatriation after myocardial infarction: a retrospective study. Heart. 2006;92(12):1864-1865.
Roby H, Lee A, Hopkins A. Safety of air travel following acute myocardial infarction. Aviat Space Environ Med. 2002;73(2):91-96.
- Zahger D, Leibowitz D, Tabb IK, et al. Long-distance air travel soon after an acute coronary syndrome: a prospective evaluation of a triage protocol. Am Heart J. 2000;140(2):241-242.
- Cox GR, Peterson J, Bouchel L, et al. Safety of commercial air travel following myocardial infarction. Aviat Space Environ Med. 1996;67(10):976-982.
Transportation Security Administration. Frequently asked questions. Accessed May 1, 2021. https://tsa.gov/travel/frequently-asked-questions
- Steven S, Frenis K, Kalinovic S, et al. Exacerbation of adverse cardiovascular effects of aircraft noise in an animal model of arterial hypertension. Redox Biol. 2020;34:101515.
Aerospace Medical Association. Ear, nose, and throat. May 2003. Accessed May 1, 2021. https://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Ear-Nose-and-Throat.pdf
Shaikh N, Wald ER, Pi M. Decongestants, antihistamines and nasal irrigation for acute sinusitis in children. Cochrane Database Syst Rev. 2014;(10):CD007909.
- Pinto JA, Dos Santos Sobreira Nunes H, Soeli Dos Santos R, et al. Otitis media with effusion in aircrew members. Aerosp Med Hum Perform. 2019;90(5):462-465.
Aerospace Medical Association. Travel with children. May 2003. Accessed May 1, 2021. https://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Travel-With-Children.pdf
Spinks A, Wasiak J. Scopolamine (hyoscine) for preventing and treating motion sickness. Cochrane Database Syst Rev. 2011;(6):CD002851.
Aerospace Medical Association. Diabetes. May 2003. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Diabetes.pdf
Passenger fitness to fly. In: Green N, Gaydos S, Hutchinson E, et al., eds. Handbook of Aviation and Space Medicine . CRC Press; 2019:263–266.
Watson HG, Baglin TP. Guidelines on travel-related venous thrombosis. Br J Haematol. 2011;152(1):31-34.
Possick SE, Barry M. Evaluation and management of the cardiovascular patient embarking on air travel. Ann Intern Med. 2004;141(2):148-154.
- Clarke MJ, Broderick C, Hopewell S, et al. Compression stockings for preventing deep vein thrombosis in airline passengers. Cochrane Database Syst Rev. 2021;(4):CD004002.
Gavish I, Brenner B. Air travel and the risk of thromboembolism. Intern Emerg Med. 2011;6(2):113-116.
Tin AH, Rabinowitz P, Fowler H. Emotional support animals: considerations for documentation. Am Fam Physician. 2020;101(5):302-304. Accessed May 1, 2021. https://www.aafp.org/afp/2020/0301/p302.html
U.S. Department of Transportation. U.S. Department of Transportation announces final rule on traveling by air with service animals. December 2, 2020. Accessed May 1, 2021. https://www.transportation.gov/briefing-room/us-department-transportation-announces-final-rule-traveling-air-service-animals
Trevorrow T. Air travel and seizure frequency for individuals with epilepsy. Seizure. 2006;15(5):320-327.
Hastings, JD; Aerospace Medical Association. Medical guidelines for airline travel: air travel for passengers with neurological conditions. September 2014. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Neurology-Sep-2014.pdf
ACOG Committee opinion no. 746: air travel during pregnancy. Obstet Gynecol. 2018;132(2):e64-e66.
Royal College of Obstetricians and Gynaecologists. Air travel and pregnancy: scientific impact paper no. 1. May 2013. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/RCOG-Pregnancy-and-Air-Travel-Scientific-Impact-Paper.pdf
Harvard Medical School. Are full-body airport scanners safe? June 2011. Accessed May 1, 2021. https://www.health.harvard.edu/diseases-and-conditions/are-full-body-airport-scanners-safe#:~:text=he%20authors%20begin%20with%20an,the%20biological%20effects%20of%20radiation
Aerospace Medical Association. Ophthalmological conditions. May 2003. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Ophthalmological-Conditions.pdf
Bettes TN, McKenas DK. Medical advice for commercial air travelers. Am Fam Physician. 1999;60(3):801-808. Accessed May 1, 2021. https://www.aafp.org/afp/1999/0901/p801.html
Aerospace Medical Association. Jet lag. May 2003. Accessed May 1, 2021. https://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Jet-Lag.pdf
Choy M, Salbu RL. Jet lag: current and potential therapies. PT. 2011;36(4):221-231.
- Waterhouse J, Reilly T, Atkinson G, et al. Jet lag: trends and coping strategies. Lancet. 2007;369(9567):1117-1129.
Herxheimer A, Petrie KJ. Melatonin for the prevention and treatment of jet lag. Cochrane Database Syst Rev. 2002;(2):CD001520.
Divers Alert Network. February 1, 2017. Accessed May 11, 2021. https://dan.org/alert-diver/article/flying-after-pool-diving-2/
Mitchell GW, Martin GJ. Chapter 19 Infectious diseases. In: Davis JR, Johnson R, Stepanek J, et al. Fundamentals of Aerospace Medicine . 4th ed. Lippincott Williams & Wilkins; 2008:432–446.
Centers for Disease Control and Prevention. Domestic travel during COVID-19. Updated April 27, 2021. Accessed April 30, 2021. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html
Co M, Ng J, Kwong A. Air travel and postoperative lymph-edema—a systematic review. Clin Breast Cancer. 2018;18(1):e151-e155.
Hu JS, Smith JK. In-flight medical emergencies. Am Fam Physician. 2021;103(9):547-552. Accessed April 30, 2021. https://www.aafp.org/afp/2021/0501/p547.html
Continue Reading

More in AFP
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Guidelines for Flying With Heart Disease
Air travel is generally safe for heart patients, with appropriate precautions
- Pre-Flight Evaluation
Planning and Prevention
During your flight.
If you have heart disease, you can fly safely as a passenger on an airplane, but you need to be aware of your risks and take necessary precautions.
Heart conditions that can lead to health emergencies when flying include coronary artery disease (CAD) , cardiac arrhythmia (irregular heart rate), recent heart surgery, an implanted heart device, heart failure , and pulmonary arterial disease.
When planning air travel, anxiety about the prevention and treatment of a heart attack on a plane or worrying about questions such as "can flying cause heart attacks" may give you the jitters. You can shrink your concern about things like fear of having a heart attack after flying by planning ahead.
Air travel does not pose major risks to most people with heart disease. But there are some aspects of flying that can be problematic when you have certain heart conditions.
When you have heart disease, air flight can lead to problems due to the confined space, low oxygen concentration, dehydration, air pressure, high altitude, and the potential for increased stress. Keep in mind some of these issues compound each other's effects on your health.
Confined Space
The prolonged lack of physical movement and dehydration on an airplane may increase your risk of blood clots, including deep vein thrombosis (DVT) or pulmonary embolism (PE) . One of the biggest risks for people with heart disease who are flying is developing venous thrombosis.
These risks are higher if you have CAD or an implanted heart device, such as an artificial heart valve or a coronary stent. And if you have an arrhythmia, a blood clot in your heart can lead to a stroke.
One of the biggest risks for people with heart disease who are flying is developing an arterial blood clot or venous thrombosis.
Low Oxygen and Air Pressure
The partial pressure of oxygen is slightly lower at high altitudes than at ground level. And, while this discrepancy on an airplane is typically inconsequential, the reduced oxygen pressure in airplane cabins can lead to less-than-optimal oxygen concentration in your body if you have heart disease.
This exacerbates the effects of pre-existing heart diseases such as CAD and pulmonary hypertension .
The changes in gas pressure in an airplane cabin can translate to changes in gas volume in the body. For some people, airplane cabin pressure causes air expansion in the lungs. This can lead to serious lung or heart damage if you are recovering from recent heart surgery.
Dehydration
Dehydration due to cabin pressure at high altitude can affect your blood pressure, causing exacerbation of heart disease. This is especially problematic if you have heart failure, CAD, or an arrhythmia.
If you experience stress due to generalized anxiety about traveling or sudden turbulence on your flight, you could have an exacerbation of your hypertension or CAD.
Pre-Flight Health Evaluation
Before you fly, talk to your healthcare provider about whether you need any pre-flight tests or medication adjustments. If your heart disease is stable and well-controlled, it is considered safe for you to travel on an airplane.
But, if you're very concerned about your health due to recent symptoms, it might be better for you to confirm that it's safe with your healthcare provider first before you book a ticket that you may have to cancel.
Indications that your heart condition is unstable include:
- Heart surgery within three months
- Chest pain or a heart attack within three months
- A stroke within six months
- Uncontrolled hypertension
- Very low blood pressure
- An irregular heart rhythm that isn't controlled
If you've had a recent heart attack, a cardiologist may suggest a stress test prior to flying.
Your healthcare provider might also check your oxygen blood saturation. Heart disease with lower than 91% O2 saturation may be associated with an increased risk of flying.
Unstable heart disease is associated with a higher risk of adverse events due to flying, and you may need to avoid flying, at least temporarily, until your condition is well controlled.
People with pacemakers or implantable defibrillators can fly safely.
As you plan your flight, you need to make sure that you do so with your heart condition in mind so you can pre-emptively minimize problems.
While it's safe for you to fly with a pacemaker or defibrillator, security equipment might interfere with your device function. Ask your healthcare provider or check with the manufacturer to see if it's safe for you to go through security.
If you need to carry any liquid medications or supplemental oxygen through security, ask your healthcare provider or pharmacist for a document explaining that you need to carry it on the plane with you.
Carry a copy of your medication list, allergies, your healthcare providers' contact information, and family members' contact information in case you have a health emergency.
To avoid unnecessary anxiety, get to the airport in plenty of time to avoid stressful rushing.
As you plan your time in-flight, be sure to take the following steps:
- Request an aisle seat if you tend to need to make frequent trips to the bathroom (a common effect of congestive heart failure ) and so you can get up and walk around periodically.
- Make sure you pack all your prescriptions within reach so you won't miss any of your scheduled doses, even if there's a delay in your flight or connections.
- Consider wearing compression socks, especially on a long trip, to help prevent blood clots in your legs.
If you have been cleared by your healthcare provider to fly, rest assured that you are at very low risk of developing a problem. You can relax and do whatever you like to do on flights—snack, read, rest, or enjoy entertainment or games.
Stay hydrated and avoid excessive alcohol and caffeine, which are both dehydrating. And, if possible, get up and walk for a few minutes every two hours on a long flight, or do leg exercises, such as pumping your calves up and down, to prevent DVT.
If you develop any concerning issues while flying, let your flight attendant know right away.
People with heart disease are at higher risk for developing severe complications from COVID-19, so it's especially important for those with heart disease to wear a mask and practice social distancing while traveling.
Warning Signs
Complications can manifest with a variety of symptoms. Many of these might not turn out to be dangerous, but getting prompt medical attention can prevent serious consequences.
Symptoms to watch for:
- Lightheadedness
- Dyspnea (shortness of breath)
- Angina (chest pain)
- Palpitations (rapid heart rate)
- Tachypnea (rapid breathing)
To prepare for health emergencies, the U.S. Federal Aviation Administration mandates that supplemental oxygen and an automated external defibrillator (AED) is on board for passenger airplanes that carry 30 passengers or more. Flight crews receive training in the management of in-flight medical emergencies and there are protocols in place for flight diversions if necessary.
A Word From Verywell
For most people who have heart disease , it is possible to fly safely as long as precautions are taken. Only 8% percent of medical emergencies in the air are cardiac events, but cardiac events are the most common in-flight medical cause of death.
This means that you don't need to avoid air travel if you have stable heart disease, but you do need to take precautions and be aware of warning signs so you can get prompt attention if you start to develop any trouble.
Hammadah M, Kindya BR, Allard‐Ratick MP, et al. Navigating air travel and cardiovascular concerns: Is the sky the limit? Clinical Cardiology . 2017;40(9):660-666. doi:10.1002/clc.22741.
Greenleaf JE, Rehrer NJ, Mohler SR, Quach DT, Evans DG. Airline chair-rest deconditioning: induction of immobilisation thromboemboli? . Sports Med. 2004;34(11):705-25.doi:10.2165/00007256-200434110-00002
American Heart Association. Travel and heart disease .
Ruskin KJ, Hernandez KA, Barash PG. Management of in-flight medical emergencies . Anesthesiology. 2008;108(4):749-55.doi:10.1097/ALN.0b013e31816725bc
Naqvi N, Doughty VL, Starling L, et al. Hypoxic challenge testing (fitness to fly) in children with complex congenital heart disease . Heart. 2018;104(16):1333-1338.doi:10.1136/heartjnl-2017-312753
By Richard N. Fogoros, MD Richard N. Fogoros, MD, is a retired professor of medicine and board-certified in internal medicine, clinical cardiology, and clinical electrophysiology.
Search for a health related topic
E.g. chlorthalidone, high blood pressure, amlodipine, can i fly on a plane if i have high blood pressure.
If you have controlled high blood pressure, you can fly on a plane. If your blood pressure is very high and uncontrolled, check with your doctor before flying. If you also have another condition such as heart or kidney failure, check with your doctor before travelling.
Whenever you travel, remember to carry your medicine in your carry-on bag. Keep an extra supply in your checked luggage in case your carry-on is lost or stolen.
You’re good to go, as long as your blood pressure is under control!

Amanda S. Carmel, M.D.
Weill cornell medicine.
.png)
Lisa Souza, M.L.I.S.
Meet our team, lifestyle changes 101--> <--.
Answer this question to help us make PALS better.
Users also read...
- How much will chlorthalidone lower my blood pressure?
- How is high blood pressure diagnosed?
Physician Recommendations
Content feedback, you rated this content less than ideal....
Please select all that apply:

See the Science
Controlled hypertension is not a contraindication to air travel as long as people are reminded to bring their antihypertensive medication with them on the flight according to the US Aerospace Medical Association Medical Guidelines for Airline Travel. 1 People with unstable medical conditions, such as uncontrolled hypertension, severe asthma, unstable angina, and severe congestive heart failure, should be evaluated by a medical professional before travel by air. 1,2 The World Health Organization (WHO) does not include hypertension as a pre-existing chronic illness that one should seek medical advice for prior to air travel. 3
WHO also recommends that travelers with a chronic illness should carry all their medications, especially prescription medications, in their carry-on luggage. 3 The medicine should be in the original containers with clear labels. People should also carry a duplicate supply of medicine in their checked baggage in case their carry-on supply is lost or stolen.
- Medical guidelines for airline travel, 2nd ed. Aviat Space Environ Med 2003; 74 (5 Suppl): A1-19.
- Thibeault C, Evans AD, Dowdall NP. AsMA medical guidelines for air travel: fitness to fly and medical clearances. Aerosp Med Hum Perform 2015; 86 (7): 656.
- World Health Organization. International travel and health: travellers with pre-existing medical conditions and special needs. http://www.who.int/ith/precautions/medical_conditions/en/ . Accessed May 20, 2018.
explanation
Can I Fly with High Blood Pressure?
by Flying Angels Editorial Team | News & Resources

An estimated 75 million people live with high blood pressure, also known as hypertension. Most of them can fly with high blood pressure as long as they remember certain safety tips that reduce the risk of any issues while traveling by plane.
The symptoms of high blood pressure can worsen at high altitudes. For example, a person with hypertension might find it more difficult to breathe on a longer flight. However, having hypertension should not become a barrier to flying. Even longer flights are fine if people take the right precautions.
As with other medical conditions such as dementia or traumatic spinal cord injury , those who want to fly with high blood pressure can choose to travel with a flight nurse who provides in-flight medical care and ensures you arrive at your destination safely.
What is Hypertension?
The term “hypertension” or high blood pressure refers to a condition where the long-term force of blood against artery walls is so high that it can lead to health problems. Most people are familiar with getting their blood pressure readings done at the doctor’s office.
Blood pressure machines provide two numbers. The top number is systolic pressure that measures pressure in the arteries when your heart beats. The bottom number is diastolic pressure that measures pressure in arteries between heartbeats.
In general, doctors consider a consistent reading of 140/90 or higher as hypertension. A normal level is generally between 90/60 and 120/80. These can vary depending on the person.
Safety Tips for Flying With High Blood Pressure
When you fly with high blood pressure, you should not worry too much about the health risks, which in itself can drive up your blood pressure! While you should always consult your physician about any concerns, most people with hypertension are perfectly safe to fly.
As Dr. Neal Chaisson with the Cleveland Clinic writes , “There’s virtually no problem with these patients traveling on a cruise, by air or even overseas.” The main issue is to stay with your medication schedule through the trip.
The doctor advises those with hypertension to carry a card that states they have pulmonary hypertension and also has their pharmacy’s number in case they lose their medication. The pharmacist should be able to help arrange a prescription refill at a nearby location. Also, make sure to bring medication in a carry-on bag, do not place it in checked baggage.
Flying with Oxygen & Medications
The following tips address things people can do during their flight.
- Stand up and move around when possible every two hours or so on longer flights
- Avoid salty snacks that can drive up blood pressure
- Sit in a way that allows for the best blood flow – do not cross your legs
- Avoid alcohol
- Take an ice pack on board to place on any areas where you begin to feel swelling, such as ankles
These tips can help avoid or relieve any symptoms you feel when you fly with high blood pressure. You also can contact a RN Flight Coordinator to find out more about how they can help you fly safely if you have hypertension.
What Should I Eat Before a Flight?
Popular Articles
- What Is Medical Escorting on Commercial Flights?
- The Skills and Equipment Needed to Manage Fragility in Medical Transport
- Challenges and Solutions in Pediatric Medical Transport
- https://www.facebook.com/FlyingAngelsInc/
- https://www.linkedin.com/company/flying-angels/
Air travel can pose health risks — even some deadly ones. Here’s what you can do to protect yourself.
- Air travel can be uncomfortable, with long hours spent in small seats, often-crummy food — if you're fed at all — and boredom. Air travel might not always be comfortable or fun, especially for frequent flyers, but it's incredibly safe.
- However, even though accidents and injuries are rare, there are a few potential health risks to be aware of when you take a flight, whether it's a short hop or a long journey.
- We spoke with three doctors to find out what you need to know to stay safe and healthy while flying.
- Sign up for Business Insider's transportation newsletter, Shifting Gears, to get more stories like this in your inbox.
- Visit Business Insider's homepage for more stories .
Catching a cold — or something else.
The most common health risk from flying: the common cold, flu, and similar viral infections.
Airplanes put a ton of people in a small enclosed space together. If someone sitting near you has a cold, there's a high chance of you being exposed to that. Especially if they're coughing and sneezing.
There's also the fact that planes aren't fully sterilized in between flights, so germs from a previous passenger could still be on surfaces like armrests or tray tables.
Compounding the problem: the stress, exhaustion, and dehydration that come with travel can make you more susceptible to catching the cold.
Dr. Umesh Gidwani, Chief of Cardiac Critical Care at The Mount Sinai Hospital, suggests that travelers worried about colds and germs bring hand sanitizer, or even cleaning wipes, on their next flight.
"You can get a pocket-sized Purell and keep your hands clean," he said.
(Disclosure: This reporter worked at the Mount Sinai Health System for several years.)
If you're especially concerned, you can also choose to wear a face mask, he said. That's especially a good option for people who might be more susceptible to catching a cold.
"People might not want to, because they find it stigmatizing, but if you're really concerned about a virus, or if it's flu season, it's always an option."
Deep-vein thrombosis.
A less common but more serious risk: deep-vein thrombosis, or DVT.
DVT is a condition that occurs when blood clots form in the large veins deep in your legs. While it can happen to virtually anyone, immobility, particularly in an upright seated position, can significantly increase the risk.
DVT doesn't just develop on flights: it can also develop on long car rides, train trips, and anywhere else that you sit for long periods of time without getting up.
"There's nothing magical about being 30,000 feet in the air," said Dr. Thomas Maldonado, Medical Director of the Venous Thromboembolic Center at NYU Langone Health. "It's more the fact that you tend to be cooped up, sedentary, immobile, and often dehydrated when you fly."
Symptoms of DVT can include aching, pain, swelling, and tightness in the leg, especially in the calf, according to Dr. Darren Schneider, Chief of Vascular and Endovascular Surgery at NewYork-Presbyterian Hospital and Weill Cornell Medicine.
In some cases, the blood clot can "chip off like a pebble in a stream and travel to the lungs," Dr. Maldonado said. That's called a pulmonary embolism, or PE, and is life-threatening. According to Dr. Maldonado, of the million Americans who are diagnosed with DVT or PE each year, about 100,000 die.
Other factors that increase your risk of developing DVT are dehydration — common on planes — smoking, genetic factors, obesity, past leg injuries, age and a history of some cancers. Another risk factor: taking hormonal birth control.
"But all these things can get magnified, or add up, traveling on a plane," Dr. Maldonado said. "So if you traveled by plane, and developed sudden pain in the calves, or swelling in the legs, that can be an important tip off."
There are a few things you can do to reduce your risk — some airlines even provide tips, Dr. Gidwani said
Leaving your seat to walk around periodically — even once every hour or so — can go a long way. Even doing exercises at your seat can help, like stretching your legs, flexing your ankles up and down, and clenching your calves.
Wearing knee-high compression socks can help, as can keeping hydrated — grabbing a large bottle of water at the airport can help with that. Avoiding alcohol can also help, Dr. Schneider said.
If you're concerned, talk to your doctor before flying. They may suggest taking an aspirin (or a baby aspirin) before your flight.
If you experience leg pain or swelling in your calf after a flight, you may have developed a DVT. Call your doctor to get it checked out.
If you develop any shortness of breath, chest pain, or sudden sharp pain, you may have a pulmonary embolism. This is a life-threatening condition, so call an ambulance or head to your nearest emergency room.
If your flight involves crossing time zones, you might experience jet lag.
Jet lag results from the body's circadian rhythm being interrupted. It most commonly causes trouble sleeping and fatigue, but can also cause minor stomach problems, anxiety and irritability, headaches, nausea, and more, according to the CDC .
The best way to manage jet lag is to try and start adjusting to your new time zone before leaving for your trip.
Make sure to be as well-rested as possible, stay hydrated, and avoid eating unhealthy foods.
Stress — and its impact on your body.
There's another issue to keep in mind.
Air travel is inherently stressful, both mentally and physically. The chaos of the airport, boarding, and getting settled; loud noise from the engines and cabin climate-control system; pressure changes as the plane climbs and descends; sodium-heavy foods; and dehydration, combined with dry cabin air, can all take a toll.
Those with existing or undiagnosed health conditions that are exacerbated by stress should be cautious. It's theoretically possible that pressure changes from takeoff and landing could also exacerbate certain heart or lung conditions, Dr. Schneider said.
"If you have severe emphysema or lung disease, like congestive heart failure, those could potentially be exacerbated by the altitude.
"People with COPD, for instance, should take special considerations with their oxygen when they fly," Dr. Gidwani added.
If you have any concerns, check with your doctor before you fly.
Also, remember that unless you have a specific health concern, getting or developing any serious health issues from a flight is extremely rare. Taking care of yourself, and making sure to move around to avoid a DVT, are the best ways to stay safe and healthy.
- Main content
Travelling with High Blood Pressure

Tommy has over 15 years experience within the insurance industry, and his primary focus is helping travellers find the right cover for their medical conditions.
Travelling with high blood pressure can be a bit stressful, especially when flying. However, with careful planning and support, travellers with high blood pressure can enjoy their holidays without any issues.
Do you or someone you know have high blood pressure? It's one of the most common long-term health conditions, affecting 1 in 3 UK adults, and it's also one of the most serious. Although it often goes symptomless, high blood pressure is a leading cause of heart attacks and strokes—accounting for 40% of all heart attacks and 60% of strokes—which is why it's often called a 'silent killer.'
The good news is that high blood pressure can be managed. As long as it's well-controlled, there's no reason you shouldn't be able to fly. Nevertheless, it's wise to be prepared and aware of potential complications while on holiday to ensure a relaxing, carefree trip. Here’s what you need to know.
What is High Blood Pressure?
Blood pressure measures the force at which your heart pumps blood throughout your body. The ideal range is between 90/60mmHg and 120/80mmHg; readings of 140/90mmHg or higher are considered elevated. While anyone can develop high blood pressure, known as hypertension, it is far more prevalent in individuals over 50.
"There are about 16 million people in the UK with high blood pressure: nine million who know they have it and seven million who don't," explains Julie Ward, Senior Cardiac Nurse at the British Heart Foundation. "Symptoms like headaches, blurred vision, or light-headedness are rare. Many have high blood pressure for years without realising it, with some only discovering it during emergencies like heart attacks or strokes."
Dr. Albert Alahmar, Consultant Interventional Cardiologist at Spire Hull and East Riding Hospital emphasises the importance of taking blood pressure medication seriously. "Hypertension is a very common condition, affecting around 20% of the population over 40. It's crucial that it is treated," he notes.
Can You Fly with High Blood Pressure?
If you have high blood pressure, the severity of your condition or the type of medication you are on could impact your ability to fly. For more information on flying and travelling with high blood pressure, visit the British Heart Foundation website.
Managing your blood pressure effectively is crucial, especially when flying. The unique conditions on an aeroplane can influence blood pressure levels. If your blood pressure is not well-controlled, or if you are pregnant and have high blood pressure, consult your doctor before making travel arrangements to ensure it is safe for you to fly.
“The atmosphere in the plane is totally different,” Dr Alahmar notes. “How we respond to that varies from one person to another, but if you measured the blood pressure of people on an aeroplane, compared to on the ground, almost certainly they will have higher blood pressure [on the plane].”
Visit Your Doctor Before Travel
If you are at all unsure about whether or not your high blood pressure might affect your holiday, it's important to take precautions. Visit your doctor before you book your trip for a quick check-up and some personalised advice. Discuss your travel plans in detail, including the destination, duration, and activities you plan to engage in.
Your doctor is the best person to determine your level of health and provide recommendations tailored to your needs. Remember that you shouldn’t travel against your doctor's advice, as doing so could put your health at serious risk. Always prioritise your well-being to ensure a safe and enjoyable holiday.
READ MORE: Fit-To-Fly Certificates

Dr Sarah Jarvis’s Top Tips
Dr Sarah Jarvis is the Clinical Director of the Patient Platform, an active medical writer, broadcaster, and the resident doctor for BBC Radio 2.
Having high blood pressure shouldn’t stop you from travelling (including by air) or enjoying a holiday if it’s controlled. However, you should speak to your doctor before you book if your blood pressure readings have been very high or unstable.
Here are some of my top tips for travelling safely if you’ve been diagnosed with high blood pressure:
- If your blood pressure is well controlled, you don’t necessarily need a blood pressure check just before you travel. However if your most recent readings have been raised, or you haven’t had a blood pressure check for over six months, see your GP or practice nurse for a reading before you travel.
- While you’re flying, avoid alcohol, keep hydrated with non-alcoholic fluids and move around the cabin regularly.
- Alcohol and exotic foods may feel like they’re an integral part of being on holiday, but remember that both alcohol and salty foods can raise your blood pressure.
- Some blood pressure medicines are diuretics – they get rid of excess fluid, bringing your blood pressure down, but these medications may make you more prone to dehydration if you’re in a very hot country or have diarrhoea and/or vomiting. Your pharmacist can advise how your blood pressure tablets work.
- Most people with high blood pressure can use saunas and hot tubs safely. However, they can cause your blood pressure to drop as blood vessels on your skin dilate to cool you down. So, look out for signs of low blood pressure, such as feeling light-headed, dizzy or faint.
If you’d like to read more of Dr Jarvis’s tips, then check out our travel insurance for high blood pressure page.
If you have started taking medication for high blood pressure in the last three months, your doctor might advise you not to travel. If you do get the green light, Ward adds: “Make sure you’ve got an adequate supply of medication so you don’t run out while you’re on holiday.”
Bringing at least an extra two weeks' worth of medication is prudent in case of loss or delays. While pharmacies are generally accessible, not all countries carry the same drug brands. Dr. Alahmar warns that switching medications abroad can be hazardous. “You don’t want to run out of tablets in a different country, as they may not have these [same] tablets. There are different families of drugs for treating high blood pressure, and we know for a fact that every patient responds to different drugs in different ways, so you may not respond to a new drug in the same way. It can be quite serious to change to different brands when you are on holiday.”
Why is Blood Pressure Medication so Important?
Lifestyle changes play an important role in managing high blood pressure, particularly keeping salt intake low, not smoking, and maintaining a healthy weight, but medication is also crucial and some people are prescribed multiple drugs. If you’ve never experienced symptoms or felt unwell, the idea of being on long-term medication can seem odd. But, as Dr Alahmar highlights, there’s been a lot of research around the effects of high blood pressure and if left untreated, “the risks of stroke and heart attacks rocket”.
An alarming proportion of people with high blood pressure are not receiving treatment. Plus, of those who have been prescribed blood pressure drugs, recent figures suggest 50-80% do not take all of their medication.
READ MORE: Travelling with Medication
This might also explain why some people don’t declare their high blood pressure when taking out travel insurance. A survey in 2014 found 1 in 20 holidaymakers aged over 50 failed to declare a medical condition in a bid to cut costs, while Foreign & Commonwealth Office figures suggest 1 in 7 holidaymakers in the over-50s bracket have travelled without insurance. According to reports, high blood pressure is the second most likely health condition people fail to declare when taking out travel insurance.
Managing Your Medication on Holiday
So, what else do you need to know about managing blood pressure on holiday? Dr Alahmar says sticking to your medication regime is vital. “Your tablets should be taken every single day – but it may be even more important to take your tablets when you travel, because of the change in conditions and the flights.”
If you are planning on travelling for a prolonged period, you might want to consider taking a blood pressure monitor with you so that you can keep an eye on your condition and keep track of any changes. It’s a good idea to chat to your Doctor about this, to find out where to get them.
Monitoring Your Blood Pressure on Holiday
Ward and Dr Alahmar both advise taking a blood pressure monitor with you on holiday. “Blood pressure machines are much easier and less expensive to buy than ever before, and if you’ve got high blood pressure, you should really be monitoring it at home and while you’re away,” says Ward. “We recommend monitoring twice a day; once in the morning, once in the evening and keep a diary. Then when you’re travelling, you can make sure it’s still OK.”
Anything from the stress of rushing through the airport, to changes in routine and climate can potentially affect your blood pressure. Foreign food can often be saltier, and Dr Alahmar notes that keeping well hydrated, especially in hot, sunny countries, is very important for people on blood pressure medication.
Sitting down to monitor your blood pressure only takes a few minutes – not a big price to pay for peace of mind. Then you can focus on the important stuff: Enjoying that well-earned break.
High Blood Pressure Travel Insurance
When travelling with high blood pressure managed by medication, it's easy to forget to declare it as a pre-existing medical condition when you buy travel insurance. However, it's crucial to remember this important step.
When telling us about your high blood pressure we’ll take you through a simple medical screening process that will help us and your travel insurance provider understand your condition and help you find the right cover to suit your individual needs.
Make Sure You’re Fully Covered
Even if your blood pressure has never caused any problems and is very well controlled, it’s crucial to declare it, along with any medication you’ve been prescribed. If you don’t and you end up falling ill and incurring costs, you may not be covered.
Every week, the Financial Ombudsman Service receives complaints from holidaymakers who’ve had travel insurance claims rejected – failure to declare pre-existing conditions is one of the most common reasons.
Your premiums won’t necessarily change very much - this will depend on other factors too, including your age, how many drugs you’re taking, and other aspects of your health history – so it’s worth comparing prices to see what travel insurance for high blood pressure options are available.
Travelling when managing high blood pressure requires careful planning and a proactive approach to ensure your well-being throughout your trip. By adhering to your medication regimen, monitoring your blood pressure regularly, and ensuring that your travel insurance fully covers your condition, you can greatly mitigate the risks associated with high blood pressure.
Remember to declare your condition and medications accurately when purchasing insurance to avoid complications. With these precautions in place, you can enjoy your holiday with peace of mind, knowing that you are prepared for any eventualities.
If you’re looking for more information and articles, be sure to check out our blog . Or, for more insurance information, take a look at our guides .
SOURCES: https://publichealthmatters.blog.gov.uk/2017/01/24/health-matters-combating-high-blood-pressure/
https://www.theguardian.com/money/2014/jul/14/best-travel-insurance-policy-pre-existing-medical-conditions
https://home.bt.com/lifestyle/money/insurance/travel-insurance-warning-to-over-50s-11363935897373
- Share this page on Facebook
- Share this page on Twitter
Sign up to receive regular updates
Get the latest news, advice, travel tips and destination inspiration straight to your inbox.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Find in topic
RELATED TOPICS
INTRODUCTION
The number of individuals exposed to high altitude through air travel and recreational activities continues to increase, with tens of millions of people traveling to high-altitude destinations each year [ 1 ]. Changes in physiologic functions during high-altitude exposure vary given an individual's physical fitness, rate of ascent, severity and/or duration of exposure, cultural habits, geographic location, and genetic variation [ 2 ]. While high altitude is well tolerated by most individuals, patients with cardiovascular disease are at risk of complications caused by tissue hypoxia and reduced oxygen delivery, sympathetic stimulation, increased myocardial demand, paradoxical vasoconstriction, and alterations in hemodynamics that occur with exposure to high altitude [ 3-5 ]. The duration of travel, ascent profile, degree of exertion, and any prior cardiovascular history can each impact the health of a patient with cardiovascular disease who is considering traveling to high altitude.
High altitude provides a unique physiologic challenge to the cardiovascular system. The cardiovascular response in both healthy individuals and in patients with cardiovascular disease will be reviewed here. Insights surrounding high-altitude disease will also be included to provide a comprehensive understanding. (See "High-altitude illness: Physiology, risk factors, and general prevention" .)
Most importantly, this topic will discuss the impact of high altitude on the heart and the associated hemodynamic changes. Altitude exposure can also lead to a variety of well-described clinical syndromes including some not directly involving the cardiovascular system, such as acute mountain sickness (AMS), high-altitude pulmonary edema, high-altitude cerebral edema, and high-altitude retinal hemorrhage. These conditions are discussed separately. (See "High-altitude pulmonary edema" and "Acute mountain sickness and high-altitude cerebral edema" and "High-altitude illness: Physiology, risk factors, and general prevention", section on 'Other altitude-related illnesses' .)
BAROMETRIC PRESSURE AND PIO2
Four key climactic indices change when moving from sea level to high altitude; atmospheric pressure, oxygen pressure, humidity, and temperature all decrease [ 4 ]. Significant changes occur beyond a critical height of 2500 meters (8200 feet) above sea level [ 6 ]. Factors such as degree of change in elevation, degree of hypoxia, rate of ascent, level of acclimatization, exercise intensity, previous history of high-altitude illness, genetics, and age significantly affect the physiologic change that the human body will experience during ascents [ 7 ]. One study involving Chinese men aged 18 to 35 years noted that increasing age (from 26 to 35 years old) was an independent risk factor for acute mountain sickness (AMS) upon rapid ascent to high altitude (from 500 to 3700 meters) and that the prevalence of AMS was more predominant with increasing age [ 8 ]. Hypoxia induces peripheral vasodilation and a pulmonary vasoconstriction, leading to changes in systemic blood pressure and an increase in pulmonary blood pressure that can also contribute to high-altitude pulmonary edema [ 9 ].
Although altitude is the most obvious determinant of barometric pressure and its resulting physiologic stress, other factors can contribute to a reduction in barometric pressure including a decrease in temperature, deteriorating weather (ie, blizzards, hail, or extreme winds), and distance from the equator.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
September 8, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Air travel may affect insulin pump delivery in people with type 1 diabetes
by Diabetologia

Altitude changes during commercial flights may affect the blood glucose levels of people with type 1 diabetes who are treated with insulin pump therapy, according to new research to be presented at this year's Annual Meeting of The European Association for the Study of Diabetes (EASD) , Madrid (9-13 Sept).
"We investigated the effect atmospheric pressure changes during flight can have on insulin pumps following concerns that glucose levels may drop below the normal ranges during or immediately after flights," explained lead author Dr. Ka Siu Fan from the Royal Surry County Hospital and University of Surrey, UK.
In the study, insulin delivery from 26 insulin pumps was tested in Europe's largest hypobaric chamber to mimic the atmospheric changes during a normal commercial flight.
The hypobaric chamber was depressurized to 550 mmHg over a 20-minute ascent, maintained at a 30-minute cruise (mimicking an airline pressurized cabin altitude of 8,000 feet), followed by a 20-minute descent to the ground (with an ambient pressure increase to 750 mmHg).
During the simulated flights, insulin infusion was set at 0.60 units per hour to represent a rate used in adult and pediatric practice and to allow accurate measurements on multiple flights.
Insulin delivery rates and bubble formation (caused by air coming out of a solution and forming bubbles when pressure decreases) were recorded by attaching infusion sets to open-ended 100 microliter capillary tubes against 1mm grid paper.
Insulin infusion sets without pumps were also tested under a separate pressure protocol to simulate rapid decompression. This mimics the sudden loss of cabin pressure, which occurs in emergencies.
The researchers found that full insulin cartridges over-delivered 0.60 units of insulin over a 20-minute ascent (ambient pressure decrease) compared to ground-level performance. While this may slightly reduce blood glucose, the authors do not anticipate that this would lead to clinically significant or symptomatic hypoglycemia.
During descent (ambient pressure increase), cartridges under-delivered 0.51 units of insulin. This may lead to blood glucose being higher than usual but does not pose the same concern as the hypoglycemic effects of too much insulin.
Strikingly, rapid decompression resulted in fluid delivery equivalent to 5.6 units of excess insulin. In the rare event of a sudden decompression of the cabin at altitude, an insulin overdose could cause blood sugar levels to fall to such an extent that it could cause significant hypoglycemia. However, in such emergencies—for instance when an aircraft loses a door mid-flight—there would be time to ingest extra short-acting carbohydrates to counter this.
As Dr. Fan explained, "Individuals who use insulin pumps should be aware of the potential impact of changes in the cabin air pressure on insulin delivery. The drop in cabin pressure during ascent may lead to a slight increase in insulin delivery as a result of the formation of air bubbles which displace excess insulin out of the cartridge.
"A slight reduction in insulin delivery is also possible during descent as the increasing air pressure dissolves the air bubbles, sucking insulin back into the pump. Whether these abnormalities in insulin delivery during flights cause clinical effects will depend on several factors, including an individual's insulin sensitivity, food intake, and glycemic control."
He cautioned, "To prevent any unintended metabolic consequences, we recommend that individuals who use insulin pumps consider temporarily disconnecting their pumps before takeoff, and removing air bubbles before reconnecting them at cruising altitude."
Explore further
Feedback to editors

Rapid blood diagnostic test developed for amyotrophic lateral sclerosis
6 hours ago

Automated insulin delivery technology helps marathon runners with type 1 diabetes
8 hours ago

Next-gen gene therapy vector for muscle diseases uses AI predictive methodology to improve efficacy and safety

Gut reaction: Low levels of manganese can aggravate inflammatory bowel disease

A novel neural explanation for choking under pressure
9 hours ago

Novel technology enabling sampling of liquids in confined spaces could aid early detection of cancer

Mouse study finds sex-based differences in how brains handle threats

A new biomarker makes it easier to distinguish between Alzheimer's and primary tauopathy
10 hours ago

Supported youth become supportive adults, researchers find
11 hours ago

Exposure to air pollution during pregnancy increases postpartum depression risk for at least three years, study finds
12 hours ago
Related Stories

Everything you need to know about insulin
Aug 31, 2024

Inhaled insulin could help people with type 1 diabetes avoid needles
Jun 24, 2024

FDA clears first automated device to deliver insulin to people with type 2 diabetes
Aug 27, 2024

Medtronic MiniMed 600 series insulin pumps recalled
Feb 15, 2020

Closed-loop insulin delivery systems may improve blood sugar control in children with type 1 diabetes
Jun 17, 2023

Glucose-responsive, charge-switchable lipid nanoparticles for insulin delivery
Apr 14, 2023
Recommended for you

Avian flu found in wastewater of 10 Texas cities through virome sequencing
15 hours ago

Conversations between clinicians and their patients about firearms could save lives
14 hours ago

Study finds doctors and patients interested in environmental impact of health care decisions
21 hours ago

Atrial fibrillation estimated to be three times more common than previously thought
Sep 11, 2024

US South Asians need targeted programs to improve heart health, study says
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
VIDEO
COMMENTS
Air travel when you have high blood pressure could lead to certain complications. Understand the risks, and learn some tips to help you have a safe flight.
A 2021 study states that people with high blood pressure can travel to high altitudes unless they have uncontrolled blood pressure or heart problems. In these situations, it is essential to talk ...
The effects of high altitude may include nausea and headaches. However, the pressurization of airplane cabins usually prevents these uncomfortable side effects. Flying with high blood pressure is possible if high blood pressure is under control. Nonetheless, anyone with high blood pressure should take the necessary precautions for air travel.
Y ou may be racking up air miles, but flying with high blood pressure could prove fatal. More than 75 million Americans are being treated for high blood pressure, according to the American Heart Association. According to The Bureau of Transportation Statistics 195 million people are flying domestically.
A person with pulmonary hypertension has high blood pressure in their lungs, causing their blood vessels to narrow and their heart to work harder. ... Air travel adds another hurdle. A plane at ...
The best way to travel with high blood pressure on an airplane is to fly with medical support. Taking a private air ambulance or traveling with a medical escort helps you access the care you need while in the air. ... You may require an air ambulance if you have high blood pressure with additional health concerns. 2. Consume Only Healthy Food ...
Detailed information on healthy considerations for air travel, including ways to prevent motion sickness and jet lag. ... If you have high blood pressure or heart problems, you should not take decongestants without the approval of your healthcare provider. Swallow often and chew gum during the flight, especially during take-off and as the plane ...
Patients with unstable angina, new cardiac or pulmonary symptoms, or recent changes in medications without appropriate follow-up should not fly until stable. 11. C. Consensus/expert opinion ...
Low Oxygen and Air Pressure . The partial pressure of oxygen is slightly lower at high altitudes than at ground level. And, while this discrepancy on an airplane is typically inconsequential, the reduced oxygen pressure in airplane cabins can lead to less-than-optimal oxygen concentration in your body if you have heart disease.
Sitting immobile on long plane flights or car, train or bus rides can slightly increase a normal person's risk of blood clots in the legs, but associated medical issues usually contribute to it. If someone has peripheral artery disease (PAD) or a history of heart failure, the clot risk increases. Recent surgery, older age and catheters in a ...
Likewise, people with difficult-to-control blood pressure, or those visiting high-altitude areas for long periods of time, may need to carefully monitor blood pressure levels for any changes. Sudden cardiac death is the most frequent non-traumatic cause of death at altitude, according to the statement.
For example, blood pressure is considered high if over 140/90mmHg, so if your blood pressure is consistently above this value then it is important to reduce it. Tips for travelling with high blood pressure: Buy travel insurance for pre-existing medical conditions to cover any high blood pressure related medical costs, should you need treatment ...
Last Updated 9/7/2018. If you have controlled high blood pressure, you can fly on a plane. If your blood pressure is very high and uncontrolled, check with your doctor before flying. If you also have another condition such as heart or kidney failure, check with your doctor before travelling. Whenever you travel, remember to carry your medicine ...
An estimated 75 million people live with high blood pressure, also known as hypertension. Most of them can fly with high blood pressure as long as they remember certain safety tips that reduce the risk of any issues while traveling by plane. The symptoms of high blood pressure can worsen at high altitudes.
However, those with high blood pressure may be at a greater risk of developing hypertension which can lead to heart failure, coronary artery disease, and other health conditions. If you suffer from high blood pressure it doesn't mean you can't travel by plane, it just means you have to be cautious.
The most common health risk from flying: the common cold, flu, and similar viral infections. Airplanes put a ton of people in a small enclosed space together. If someone sitting near you has a ...
Experts advise people with heart conditions or high blood pressure consult a health care professional before traveling to higher altitudes to develop a plan for safe travel and what to do in case of an emergency. ... place unique challenges on the heart and blood vessels due to lower levels of oxygen and fluctuations in air pressure ...
Blood pressure measures the force at which your heart pumps blood throughout your body. The ideal range is between 90/60mmHg and 120/80mmHg; readings of 140/90mmHg or higher are considered elevated. While anyone can develop high blood pressure, known as hypertension, it is far more prevalent in individuals over 50.
I would love to go, but I have high blood pressure and worry that high altitudes are dangerous for people with high blood pressure. Is that the case? A. If you have high blood pressure but are otherwise healthy, your blood pressure is under control, and you take some precautions, a trip to the Rocky Mountains should be fine.
FAQ. Summary. Flying can cause temporary effects, such as ear discomfort, jet lag, and dehydration. It can also increase the risk of deep vein thrombosis (DVT). However, many people take flights ...
INTRODUCTION. The number of individuals exposed to high altitude through air travel and recreational activities continues to increase, with tens of millions of people traveling to high-altitude destinations each year [].Changes in physiologic functions during high-altitude exposure vary given an individual's physical fitness, rate of ascent, severity and/or duration of exposure, cultural ...
It empties your energy tank. Air pressure is lower at higher altitudes, which means your body takes in less oxygen. Airlines "pressurize" the air in the cabin, but not to sea-level pressures ...
Selecting the right compression socks is crucial for their effectiveness. Here are some tips: Choose the Right Compression Level: Compression socks come in various pressure levels, measured in millimeters of mercury (mmHg). For flying, moderate compression (15-20 mmHg) is generally sufficient, but higher levels may be recommended by a healthcare provider if you have specific health conditions.
High Blood Pressure; Artificial Intelligence; Lung Cancer; ... One important current issue is that of the spread of infectious diseases through air travel. 2014 saw over 3.3 billion passengers ...
Baggage claim low: If you wear a pump while flying, make sure to double-check your blood sugar after landing. The quick change in altitude (and air pressure) can impact the rate that your pump administers insulin when the plane is taking off and landing, which often leads to low blood sugar for people by the time they reach baggage claim.
Altitude changes during commercial flights may affect the blood glucose levels of people with type 1 diabetes who are treated with insulin pump therapy, according to new research to be presented ...
Deep vein thrombosis can be a serious health issue that strikes at any time. But medium-to long-haul flights increase the risk of developing it.