
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Info

Fever Blisters & Canker Sores
Both fever blisters and canker sores are common across all ages and can be painful. However, they are separate conditions with different causes. Read further to learn how to tell them apart and find out which treatments might help ease the pain.
Fever Blisters (also known as cold sores) are painful fluid-filled sores that form on the outside of the mouth around the lips. Fever blisters are very contagious.
Canker Sores are painful white or yellow sores that only form inside the mouth, usually on the insides of the cheeks or lips or on the tongue. Canker sores (also called aphthous ulcers ) are not contagious.
Fever Blisters are caused by an infection with the herpes simplex virus, usually type 1, or HSV-1. It is estimated that nearly 90 percent of U.S. adults have been infected with the virus, although many people with the infection do not ever show symptoms. The virus generally resides in the nerve cells where it may periodically reactivate, traveling to the skin and causing recurring fever blisters.
Canker Sores do not have a known cause. They may be triggered by an injury, stress, smoking, or deficiencies in folic acid, iron, or vitamin B12.
Symptoms of fever blisters:
- Fluid-filled blisters on the outside of the mouth around the lips.
- Burning or tingling sensation at the site where the blisters will appear.
- And sometimes, fever, fatigue, or swelling of the lymph nodes, similar to other viral infections.
Symptoms of canker sores :
- A round white or yellow sore with a red border inside the mouth, usually on the inside of the lips or cheeks or on the tongue.
- A burning or tingling sensation may occur in the mouth prior to the formation of the sore.
The main way to tell the difference between a fever blister and a canker sore is by location. Fever blisters occur outside the mouth, generally around the border of the lips. Canker sores occur inside the mouth.
They also differ in appearance: Fever blisters are patches of several small fluid-filled blisters, while canker sores are usually single round white or yellow sores with a red border.
Typically, both types of sores go away on their own and treatment is not usually required. There is no known treatment that can permanently cure fever blisters or canker sores and prevent them from recurring. Treatment focuses on minimizing the pain and speeding recovery time.
Fever blisters can be treated with prescription antiviral medications either applied as topical creams or taken orally. See a doctor if your cold sores persist longer than a few weeks, you develop a high fever, or you notice eye irritation.
Canker Sores can be treated with over-the-counter (non-prescription) gels to numb the pain. Avoiding spicy or abrasive foods may also help. Rinsing the mouth with over-the-counter antiseptic medications may help prevent infection of the sore and speed healing.
See a doctor if you have frequently recurring canker sores or if the sores are severe enough to make eating or drinking difficult. If you have recurring canker sores as a result of a vitamin deficiency, treating the deficiency may reduce their frequency.
Helpful Tips
Both fever blisters and canker sores can have triggers that produce flare ups. Try to identify and then avoid triggers so your flare ups become less frequent.
Tips for Fever Blisters
- Sun exposure may sometimes trigger outbreaks of fever blisters. If you have recurring blisters, using sunscreen may help reduce their frequency.
- Fever blisters are contagious. Avoid kissing, sharing eating utensils, cups, water bottles, or other items if you are experiencing symptoms.
- Be aware that in young children, fever blisters can cause loss of appetite, drooling, and fever that can last for several days.
- Talk to your doctor or your child’s pediatrician if symptoms are severe or recur frequently.
Tips for Canker Sores
- If you regularly get canker sores, talk to your doctor about testing for food allergies, as allergic reactions can sometimes trigger canker sore outbreaks.
Additional Resources
- MedlinePlus (Fever Blisters) Information about oral herpes (the infection that causes cold sores) from the NIH National Library of Medicine.
- MedlinePlus (Canker Sores) Information about canker sores from the NIH National Library of Medicine.
- Patient Care & Health Information
- Diseases & Conditions

Illustration of cold sore on different skin colors. A cold sore is a cluster of fluid-filled blisters. Healing often occurs in two to three weeks without scarring. Cold sores are sometimes called fever blisters.
Cold sores, or fever blisters, are a common viral infection. They are tiny, fluid-filled blisters on and around the lips. These blisters are often grouped together in patches. After the blisters break, a scab forms that can last several days. Cold sores usually heal in 2 to 3 weeks without leaving a scar.
Cold sores spread from person to person by close contact, such as kissing. They're usually caused by herpes simplex virus type 1 (HSV-1), and less commonly herpes simplex virus type 2 (HSV-2). Both of these viruses can affect the mouth or genitals and can be spread by oral sex. The virus can spread even if you don't see the sores.
There's no cure for cold sores, but treatment can help manage outbreaks. Prescription antiviral medicine or creams can help sores heal more quickly. And they may make future outbreaks happen less often and be shorter and less serious.
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
A cold sore usually passes through several stages:
- Tingling and itching. Many people feel itching, burning or tingling around the lips for a day or so before a small, hard, painful spot appears and blisters form.
- Blisters. Small fluid-filled blisters often form along the border of the lips. Sometimes they appear around the nose or cheeks or inside the mouth.
- Oozing and crusting. The small blisters may merge and then burst. This can leave shallow open sores that ooze and crust over.
Symptoms vary, depending on whether this is your first outbreak or a recurrence. The first time you have a cold sore, symptoms may not start for up to 20 days after you were first exposed to the virus. The sores can last several days. And the blisters can take 2 to 3 weeks to heal completely. If blisters return, they'll often appear at the same spot each time and tend to be less severe than the first outbreak.
In a first-time outbreak, you also might experience:
- Painful gums.
- Sore throat.
- Muscle aches.
- Swollen lymph nodes.
Children under 5 years old may have cold sores inside their mouths. These sores are often mistaken for canker sores. Canker sores involve only the mucous membrane and aren't caused by the herpes simplex virus.
When to see a doctor
Cold sores generally clear up without treatment. See your health care provider if:
- You have a weak immune system.
- The cold sores don't heal within two weeks.
- Symptoms are severe.
- The cold sores often return.
- You have gritty or painful eyes.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Cold sores are caused by certain strains of the herpes simplex virus (HSV). HSV-1 usually causes cold sores. HSV-2 is often the cause of genital herpes. But either type can spread to the face or genitals through close contact, such as kissing or oral sex. Shared eating utensils, razors and towels can also spread HSV-1 .
Cold sores are most likely to spread when you have oozing blisters. But you can spread the virus even if you don't have blisters. Many people who are infected with the virus that causes cold sores never develop symptoms.
Once you've had a herpes infection, the virus can hide in nerve cells in the skin and may cause another cold sore at the same place as before. A return of cold sores may be triggered by:
- Viral infection or fever.
- Hormonal changes, such as those related to a menstrual period.
- Being in the sun or wind.
- Changes in the immune system.
- Injury to the skin.
- Video: 3 things you didn't know about cold sores
Ian Roth: Cold sores on the lips can be embarrassing and tough to hide. But, turns out, you might not have a reason to be embarrassed.
Pritish Tosh, M.D., Infectious Diseases, Mayo Clinic: About 70-plus percent of the U.S. population has been infected with herpes simplex 1. Now, a very small percentage of those people will actually develop cold sores.
Ian Roth: Dr. Pritish Tosh, an infectious diseases specialist at Mayo Clinic, says genetics determines whether a person will develop cold sores.
Dr. Tosh: A proportion of the population, they don't quite have the right immunologic genes and things like that and so they're not able to handle the virus as well as other people in the population.
Ian Roth: The problem is people can spread the herpes virus whether they develop cold sores or not. Herpes virus spreads through physical contact like kissing, sharing a toothbrush — even sharing a drinking glass — or through sexual contact.
Dr. Tosh: Since the number of people who are infected but don't have symptoms vastly outnumber the people who are infected and have symptoms, most new transmissions occur from people who have no idea that they are infected.
For the Mayo Clinic News Network, I'm Ian Roth.
Risk factors
Almost everyone is at risk of cold sores. Most adults carry the virus that causes cold sores, even if they've never had symptoms.
You're most at risk of complications from the virus if you have a weak immune system from conditions and treatments such as:
- HIV / AIDS .
- Atopic dermatitis (eczema).
- Cancer chemotherapy.
- Anti-rejection medicine for organ transplants.
Complications
In some people, the virus that causes cold sores can cause problems in other areas of the body, including:
- Fingertips. Both HSV-1 and HSV-2 can be spread to the fingers. This type of infection is often referred to as herpes whitlow. Children who suck their thumbs may transfer the infection from their mouths to their thumbs.
- Eyes. The virus can sometimes cause eye infection. Repeated infections can cause scarring and injury, which may lead to vision problems or loss of vision.
- Widespread areas of skin. People who have a skin condition called atopic dermatitis (eczema) are at higher risk of cold sores spreading all across their bodies. This can become a medical emergency.
Your health care provider may prescribe an antiviral medicine for you to take on a regular basis if you develop cold sores more than nine times a year or if you're at high risk of serious complications. If sunlight seems to trigger your condition, apply sunblock to the spot where the cold sore tends to form. Or talk with your health care provider about using an oral antiviral medicine before you do an activity that tends to cause a cold sore to return.
Take these steps to help avoid spreading cold sores to other people:
- Avoid kissing and skin contact with people while blisters are present. The virus spreads most easily when the blisters leak fluid.
- Avoid sharing items. Utensils, towels, lip balm and other personal items can spread the virus when blisters are present.
- Keep your hands clean. When you have a cold sore, wash your hands carefully before touching yourself and other people, especially babies.
- AskMayoExpert. Cold sores (herpes simplex infection). Mayo Clinic; 2019.
- Dinulos JGH. Warts, herpes simplex, and other viral infections. In: Habif's Clinical Dermatology. 7th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed April 7, 2020.
- Herpes simplex. American Academy of Dermatology. https://www.aad.org/public/diseases/a-z/herpes-simplex-overview. Accessed April 7, 2020.
- Ferri FF, et al., eds. Herpes simplex. In: Ferri's Fast Facts in Dermatology: A Practical Guide to Skin Diseases and Disorders. 2nd ed. Elsevier; 2019. https://www.clinicalkey.com. Accessed April 7, 2020.
- Kermott CA, et al., eds. Canker sores. In: Mayo Clinic Book of Home Remedies. 2nd ed. Time; 2017.
- Kermott CA, et al., eds. Cold sores. In: Mayo Clinic Book of Home Remedies. 2nd ed. Time; 2017.
- Gibson LE (expert opinion). Mayo Clinic. April 6, 2015.
- Lemon balm. Natural Medicines. https://naturalmedicines.therapeuticresearch.com/. Accessed April 8, 2020.
- Lysine. Natural Medicines. https://naturalmedicines.therapeuticresearch.com/. Accessed April 8, 2020.
- Rhubarb. Natural Medicines. https://naturalmedicines.therapeuticresearch.com/. Accessed April 8, 2020.
- Propolis. Natural Medicines. https://naturalmedicines.therapeuticresearch.com/. Accessed April 8, 2020.
- Bauer BA, ed. Making wellness the focus of care. In: Mayo Clinic Guide to Integrative Medicine. Time; 2017.
- Klein RS. Treatment of herpes simplex virus type 1 infection in immunocompetent patients. https://www.uptodate.com/contents/search. Accessed April 8, 2020.
- Hargitai IA. Painful oral lesions. Dental Clinics of North America. 2018; doi.10.1016/j.cden.2018.06.002.
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
5 Stages of Cold Sores and What to Do

In this article
5 Stages of a Cold Sore (How They Form)
Not everyone with cold sores experiences the same set of symptoms or symptoms in the same order.
But there are 5 distinct cold sore stages. A cold sore is contagious from the time you first experience symptoms until it’s completely healed.
Typical cold sore stages include:
Stage 1: Tingling
During this cold sore stage, many people feel an odd sensation where a cold sore develops 12 to 24 hours before they’re noticeable.
Some people describe this sensation as:
- Tingling with numbness
The skin often becomes red, inflamed, and painful as blisters form. It can also become dry and itchy.
People who experience these early symptoms or warning signs of cold sores may never actually have a cold sore outbreak. Applying OTC antiviral ointments for cold sores or taking prescription antiviral medications at this stage may prevent them from forming and improve the healing process.
During first outbreaks, it can take up to 20 days for symptoms to develop after being exposed to the cold sore virus.
Stage 2: Blistering
Tiny, painful, fluid-filled blisters begin to form. Blisters may appear alone or as multiple blisters close together in groups or patches.
At first, a cold sore blister appears clear, then becomes pus-filled and cloudy during this stage. The skin blisters and underneath is typically redder than usual. Do not try to pop, irritate, or break open blisters.
Cold sores typically develop on the lips or around the mouth. But a cold sore can form on the nose, cheeks, and other body parts. Talk to a doctor if cold sores develop on the genitals.
Sores may also develop in the mouth during your first outbreak.
In rare cases, cold sores impact the eyes. Without proper, early treatment, herpes eye infections can affect your eyesight.
Seek immediate medical attention if a cold sore develops near or on the eye, or the eyes become:
- Sensitive to light
Stage 3: Weeping
Cold sore blisters burst and leak, or weep, clear to yellowish-colored fluid for a few days. Sometimes blisters merge before they rupture.
Blisters tend to rupture 2 to 3 days after they develop or 48 hours after warning symptoms develop.
Once they rupture, blisters leave behind shallow, red, exposed, and ulcerated sores. The skin around the sores is often painful, dry, and irritated during this period.
Cold sores are most contagious during the weeping stage. Avoid picking or touching weeping sores to prevent them from worsening, spreading, or becoming infected with bacteria.
Stage 4: Crusting
Like other wounds, after cold sore blisters rupture, they crust and form scabs. Crusting and scabbing typically occur 4 to 5 days after cold sores appear. Scabs may crack or bleed a bit as they heal.
Do not try to pick or pull off scabs or crusting. Applying hydrating creams or ointments can help scabs from becoming too itchy.
Stage 5: Healing
During the final stage of a cold sore, scabs fall or flake off on their own after a few days. The skin underneath scabs tends to be redder, pinker, or more sensitive than normal. It often takes 1 to 3 weeks for sores to heal completely.
Most cold sores don’t leave permanent scars unless they’re severe or extensive. But scabs are often painful and irritating during this stage.
What Causes Cold Sores?
Cold sores are tiny, fluid-filled blisters that usually form on the lips. They are also called fever blisters or oral herpes.
Cold sores are contagious and spread through close contact with bodily fluids or secretions. They are most contagious when the blisters are oozing, but can spread even when invisible.
The herpes simplex virus 1 (HSV-1) causes most cold sores. But the herpes simplex virus 2 (HSV-2) can also cause it. More than 50% of people in the U.S. have the cold sore virus.
After a cold sore heals, the herpes simplex virus becomes dormant (inactive) and lives in nerve cells. Certain factors can trigger the herpes virus to reactivate and cause sores, typically in the same place as before.
Common triggers for cold sores include:
- Sunlight, wind, and cold weather
- Immune changes
- Menstruation
- Dry, damaged, or cracked lips
- Certain foods
- Dental work
- Cosmetic procedures
- Gastrointestinal problems
Common Symptoms
Only around 20 to 40% of people infected with herpes develop cold sores. People usually develop different symptoms depending on whether it’s their first cold sore outbreak.
During your first outbreak, you may experience the following initial symptoms for 1 to 2 weeks:
- A burning sensation in the mouth followed by the formation of painful sores on the lips, gums, tongue, or throat
- Sore throat and pain when swallowing
- Painful gums
- Red or swollen gums
- Muscle aches
- Swollen lymph nodes
During subsequent herpes outbreaks, most people develop painful, hard blisters that ooze clear or yellow fluid once they burst.
How Long Do Cold Sores Last?
Cold sores normally last several days before rupturing and forming a scab. Most cold sore scabs take 1 to 3 weeks to heal completely.
If cold sores are recurring, they are often less severe and only take a week to heal.
When to See a Doctor for a Cold Sore
Most cold sores don’t require medical attention.
Talk to a doctor if you have:
- Cold sores that don’t heal after 2 to 3 weeks
- An immune condition or weakened immune system
- Severe symptoms or frequent, large, or numerous cold sores
- Cold sores on the eyes, genitals, or other body parts
- A fever, spreading redness, or discolored pus
A doctor will typically diagnose a cold sore by looking at it. They may also take a swab of the sore and send it away for testing.
Medical Treatments
There’s no cure for herpes, but some medications can help reduce symptoms and speed up healing.
People with frequent cold sores or a high risk of complications can take antiviral medication routinely or before exposure to triggers. If oral antibiotics are not effective, you can take antiviral medications intravenously (IV).
Home Remedies
Some at-home remedies can reduce cold sore symptoms and improve the healing process.
At-home remedies for cold sores include:
- Applying cold compresses
- Taking oral OTC pain or anti-inflammatory medications, but not aspirin
- Applying OTC topical treatments with numbing agents, like lidocaine, by using a clean Q-tip or cotton swab
- Consuming cold, soft foods and drinks
- Avoiding acidic, salty, or spicy foods
- Applying sunscreen or lip balm with SPF
- Avoiding or limiting exposure to triggers
- Managing stress
- Not touching cold sores
- Applying OTC cold sore patches that protect the skin during healing
- Drinking plenty of fluids to prevent dehydration
- Applying zinc ointments or creams to scabs
- Washing your hands frequently
Some OTC creams and ointments can prevent cold sores if you apply them before they appear (when warning signs develop). They can also improve healing.
Prevention Tips
There are steps you can take to reduce the risk of being infected with the herpes virus. There are also ways to prevent cold sores and recurrent outbreaks.
Common tips include:
- Avoid skin-to-skin or intimate contact with someone with cold sores
- Wash your hands before touching yourself or others when you have cold sores
- Avoid sharing personal items, such as those that touch the skin
- Get enough sleep
- Protect your skin from harsh sun, wind, or cold
- Maintain a healthy, balanced diet
- Avoid contact with sick people
Share this article
Related pages.

Medically Reviewed by Erica Anand

Oral Herpes - Causes, Symptoms & Treatments
Medically Reviewed by Khushbu Gopalakrishnan

Is That a Blood Blister in Your Mouth?

9 Best Cold Sore Treatments for Fast Relief
Medically Reviewed by Nandita Lilly

Mouth Sores
Medically Reviewed by Elena Borrelli

5 Possible Causes of Roof of Mouth Pain & Their Treatments
- American Academy of Dermatology Association “ Cold sores: Overview. ” American Academy of Dermatology Association
- Ceders Sinai “ Cold sores. ” Cedars Sinai
- Cleveland Clinic “ Cold sores. ” Cleveland Clinic
- Johns Hopkins Medicine “ Cold sores .” Johns Hopkins Medicine.
- Mayo Clinic “ Cold sores. ” Mayo Clinic
- National Health Service “ Cold Sores. ” National Health Service.
- Nemours Teens Health “ Cold sores(HSV-1). ” Nemours Teens Health
- StatPearls “ Herpes Simplex Type 1. ” StatPearls
- University of Michigan Health Service “ Cold and canker sores. ” University of Michigan Health Service

- 717.243.9020
- Appointment Request

- William Noll, DMD
- Devin Caster, DMD, FAGD
- Cali Coble, DMD
- Restorative Team
- Hygiene Team
- Administrative Team
- New Patients
- Accepted Insurance Plans
- Your First Visit
- Pay My Bill
- Financial Information
- Refer A Friend
- Dental Cleanings
- Teeth Whitening
- Gum Disease Treatment
- Smile Restoration
- Cosmetic Dentistry
- Dental Implants
- Root Canal Therapy
- TMJ Treatment
- Dental Sealants
- Crooked Teeth
- Invisalign Treatment
- Orthodontist in Carlisle, PA
- Pediatric Dentistry
- Your Child's First Visit
- Dental X-Rays for Children
- Bruxism in Children
- How Baby Teeth Affect Permanent Teeth
Carlisle's Dental Health Blog

Can I go to the dentist if I have cold sores?
As your stare into the mirror examining the sore on your lip, you realize you have your next cleaning with your dentist coming up. You’ve gotten these sores in the past and know that it’s a cold sore. You also know that the virus that causes cold sores is incredibly contagious, so what do you do? Your smile is important to you and you wouldn’t want to put that at risk. Is a visit worth the potential to spread the virus? The short answer is no, at least not most of the time.
What is a cold sore?
As you may already know, cold sores are a group of tiny, painful blisters that are caused by the herpes simplex virus (HSV). The symptoms you experience are usually the most severe the first time you get a cold sore. Once a cold sore has broken out, your body will usually make antibodies and you might not get another infection. Despite this, it is possible for them to return. They’ll usually appear on the outside of the mouth and lips, but it’s possible for them to show up on the nose and cheeks. Certain things can trigger an outbreak to occur, such as:
- Certain foods
- Sunburn or being in strong sunlight
- Dental work or cosmetic surgery
- Menstruation
For most people having a cold sore outbreak is just an inconvenience and something to be mindful of to prevent the spread. The spread of HSV can occur from kissing someone who has the virus, sharing eating utensils, towels, or razors. Some people with compromised immune systems may need extra care if they develop a cold sore.
Should I keep my appointment?
Given the high transmissibility of HSV, is it wise to go to your dentist? The best thing to do is to call your dentist and ask, but more than likely you’ll be asked to come back at a different time. Even though your dentist will wear gloves while they examine you, it’s still very possible to spread this highly contagious virus. Prior to the healing process that the cold sore goes through, you’re most contagious. Some dentists, however, will begin seeing people with cold sores again after that healing process has started and the sores have begun to scab. Even after that point, some people may experience pain from the dried-out sores. It might be hard to keep your mouth open for extended periods. This is perfectly normal and your dentist would understand if you needed to wait a little longer for the scab to fall off entirely.
Since these sores could easily spread to your dentist or the hygienist, it’s usually best to talk with them to make a plan for rescheduling your appointment once your cold sore has subsided. You want to ensure the safety and health of everyone at your dentist’s office. It’s best to determine where you’re at in the healing process and to give your dentist a call to see what they think.
- Address: 701 S West Street, Carlisle, PA 17013 Get Directions
- Phone: + 1 (717) 243 9020
- Email: [email protected]
We're proud to provide extraordinary dental care in Carlisle , Boiling Springs , & Newville, PA.
Find a Registered Dental Hygienist
Knowledge network, fact sheet: herpes simplex infection (various intra- or peri-oral infections/manifestations also known as herpetic gingivostomatitis, herpes labialis, herpes simplex labialis, oral herpes, cold sore, and fever blister; finger infection known as herpetic whitlow; caused by herpes simplex virus type 1 [hsv-1] and less commonly by herpes simplex virus type 2 [hsv-2]), is the initiation of non-invasive dental hygiene procedures* contra-indicated, is the initiation of invasive dental hygiene procedures contra-indicated**, oral management implications, oral manifestations, related signs and symptoms, references and sources of more detailed information, is the initiation of non-invasive dental hygiene procedures* contra-indicated.
- Yes, if the patient/client has potentially contagious lesions in or near the mouth, whether from primary herpetic gingivostomatitis or from recurrent oral herpes simplex. Other than oral hygiene instruction, professional care should not be performed until the vesicles/ulcers have completely healed, because of the risk of transmission of the virus to other head and neck areas of the patient/client or to the dental hygienist.
Is medical consult advised?
- Yes, to obtain a definitive diagnosis from a physician or dentist in the case of primary herpetic gingivostomatitis (and associated supportive management) or, in the case of recurrent oral herpes, to potentially obtain antiviral therapy to reduce pain and duration of symptoms.
Is the initiation of invasive dental hygiene procedures contra-indicated?**
- Yes. See above.
Is medical consult advised?
Is medical clearance required?
Is antibiotic prophylaxis required?
Is postponing treatment advised?
- Yes, elective oral care should be postponed until oral and facial lesions of the patient/client have completely healed.
Oral management implications
- Mode of transmission of HSV-1 is primarily via contact with the saliva of carriers, resulting in oral herpes. Transmission may also occur via contact of active cold sores on the lips of carriers or via contact with other active herpetic lesions. Less commonly, according to some sources, herpes virus may also be transmitted via touching objects that are infected with the virus, including infected razors, towels, dishes, and other shared items. Transmission of HSV-2 is usually via sexual contact and causes genital herpes. However, oral-genital, oral-anal or anal-genital contact means that HSV-1 and HSV-2 may be transmitted to various sites, and the historical distinction between the two types of HSV in terms of site of infection is now blurred. After the initial infection, the virus becomes dormant in the sensory ganglia of the face (or genital area); reactivation of the virus causes cold sores of the mouth (or genital sores, if the primary infection was in the genital area).
- Routine barrier infection control measures (i.e., mask, eye protection, and gloves) are essential in reducing the transmission of the herpes simplex virus to oral health care providers.
- Patients/clients with primary herpetic gingivostomatitis (PHGS) should be advised to rest, drink fluids, and eat soft, nutrient-rich foods. Teeth can be cleaned at home with an extra-soft toothbrush if tolerated. Over-the-counter topical anaesthetics and systemic nonsteroidal anti-inflammatory drugs (NSAIDs) can be used to minimize discomfort. However, topical anaesthetics should be used cautiously with children in order not to anaesthetize the throat, which can be distressing.
- Pain associated with oropharyngeal HSV lesions of PHGS can significantly restrict the patient/client’s intake of food, thereby potentially compromising adequate nutrition.
- Even if the dental hygienist has been previously exposed to the herpes virus (which is highly probable) or has had a symptomatic initial infection with or without recurrent lesions, the hygienist can still be inoculated with HSV by inadvertent finger puncture with a virus-contaminated instrument. This can result in herpetic whitlow , which is a potentially recurrent herpetic lesion of the finger that can be very painful and debilitating.
- Patients/clients with recurrent (secondary) oral herpes simplex infections (i.e., cold sores) may be advised to apply ice or a warm washcloth to the lesions for pain relief; wash the blister gently with antiseptic soap and water to reduce potential virus to other body areas; avoid hot beverages, spicy and salty foods, and citrus fruits/juices; gargle with cool water; rinse with salt water; and take a pain reliever such as acetaminophen or ibuprofen. Referral to a physician or dentist is appropriate for consideration of treatment with prescription antiviral agents, with oral medications generally working better than topical formulations. Antiviral medications such as acyclovir, famciclovir, and valacyclovir work best if used during the prodromal (tingling/burning) phase, before any blisters develop. For patients/clients with very frequent recurrences, prophylactic continual use of antivirals may be a consideration.
- Recurrent herpes simplex lesions shed huge amounts of herpes virus, and thus the dental hygienist should not treat the patient/client who has orofacial lesions. Not only are herpetic whitlow lesions a possibility from virus transmission from the patient/client to the dental hygienist, but the virus is also shed in the saliva, and thus spatter during treatment can be hazardous.
- Patients/clients with recurrent oral herpes simplex should be educated about their condition and how to prevent spread of infection. Persons with frequent recurrences are often attuned to the prodromal symptoms, and they should be instructed to reschedule dental hygiene appointments until the episode has run its course.
- The use of sunscreens may reduce the recurrence of herpes labialis in some patients/clients.
- If you, the dental hygienist, have a herpetic whitlow lesion on your hand, you should not engage in patient/client contact until it has completely healed, because you pose an infectious risk to others. Gloves are insufficient protection. Herpetic whitlow of the hand/fingers can last many weeks longer than the usual two weeks or so course of active herpes virus infection in the oral tissue.
- If you, the dental hygienist, have active cold sores (i.e., active primary or recurrent herpetic lesions on the face), you should exercise meticulous infection control (including covering of lesions) when performing procedures involving close proximity to patients/clients. For patients/clients particularly susceptible to infection (e.g., those who are significantly immunocompromised , consideration should be given to deferring elective care until your lesions have healed.
Oral manifestations
- Primary herpetic gingivostomatitis (PHGS) typically occurs following first-time exposure of seronegative persons or those who have not produced adequate antibody response during a previous infection with either of the two HSVs. PHGS typically affects children between the ages of 6 months and 6 years, and may be mild or severe. Many infections are subclinical, with infected persons exhibiting no signs or symptoms. While initial oral infection with HSV-1 usually occurs before the sixth year of life, primary infections in adults are increasingly being reported.
- PHGS is characterized by oral and/or perioral vesiculoulcerative lesions. While herpetic gingivostomatitis is a self-limiting disease, affected persons may experience severe pain that constrains eating and drinking. Symptoms usually appear between 1 to 3 weeks after initial contact with the virus, and may last up to 3 weeks.
- Symptomatic PHGS is usually preceded or accompanied by a burning or tingling sensation at the site of inoculation, cervical and submandibular lymphadenopathy, sore throat, fever, malaise, myalgia, headache, decreased appetite, and pain with swallowing. The characteristic vesicular eruptions may occur on the skin, vermilion border of the lips, or on any mucosal surface intraorally. The discrete, grayish vesicles typically rupture and coalesce within 24 hours to form ulcers with a red, elevated “halo” margin with a depressed gray or yellow central area. The ulcers teem with shedding virus.
- In healthy persons, recovery from primary infection is expected within 7 to 14 days. Only 15% to 40% of seropositive patients/clients go on to experience recurrent mucocutaneous lesions.
- Recurrent (secondary) oral herpetic infection may be triggered by emotional stress, fatigue, fever, sun exposure, onset of menses, illness, and physical trauma. Patients/clients often have prodromal symptoms of pain, burning or tingling at the site where the lesion recurs. Within several hours of the prodrome, vesicles appear, which then become ulcerated and coalesce into a large ulcer or ulcer, typically on the lip or perioral skin. The lesions may be painful, and they crust over as healing occurs. Healing occurs without scarring in about 14 days. Recurrences may be rare, or may occur as often as monthly. Lesions usually recur in the same place on the vermilion border or skin around the face, and recurrent symptoms are usually milder than those associated with the initial episode.
- Recurrent herpetic lesions can occur intraorally — typically on keratinized mucosa of the hard palate or gingiva — as well as on the lips. This distinguishes them from the more commonly occurring aphthous ulcers, which usually appear on the movable mucosa. Dental procedures frequently induce intraoral herpes recurrence on the epithelium adjacent to the teeth.
- In some persons, HSV is present in the oral cavity, even when no lesions are present.
Related signs and symptoms
- Herpes simplex is a viral infection characterized by a localized primary lesion, latency in nerve tissue (e.g., trigeminal, facial, and vagus ganglia), and a tendency to local recurrence. Irrespective of the viral type, HSV primarily affects the mucous membranes and skin. The two causal agents — HSV-1 and HSV-2 — generally produce distinct clinical syndromes, depending on the portal of entry. Either may infect the oral mucosa (oral herpes) or genital tract (genital herpes).
- The prevalence of HSV-1 infection increases gradually from childhood, with up to 90% of the population developing antibodies to HSV-1. Most people in Canada are infected with oral HSV-1 by 20 years of age.
- Unusual manifestations of primary herpetic infection may include non-perioral facial skin (e.g., near the eye). Meningoencephalitis may also occur.
- Herpetic infection of the cornea (i.e., herpetic keratitis) is a serious condition. Recurrences are extremely painful and may last months. Partial loss of sight can occur.
- Neonatal primary infection with HSV can result in fatal generalized infections of newborns infants via viral transmission from the birth canal or, less commonly, via intrauterine transmission. Neonatal risk is elevated if the mother is undergoing primary infection herself.
References and sources of more detailed information
- Laheij AM, Kistler JO, Belibasakis GN, Välimaa H, de Soet JJ; European Oral Microbiology Workshop (EOMW) 2011. Healthcare-associated viral and bacterial infections in dentistry. J Oral Microbiol. 2012;4:10.3402/jom.v4i0.17659. doi:10.3402/jom.v4i0.17659 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3375115/
- Raborn GW and Grace MGA. Recurrent Herpes Simplex Labialis: Selected Therapeutic Options. J Can Dent Assoc 2003;69(8):498-503. http://www.cda-adc.ca/jcda/vol-69/issue-8/498.pdf
- RDH Magazine https://www.rdhmag.com/infection-control/article/16406510/infection-control-and-herpes-simplex
- Today’s RDH https://www.todaysrdh.com/why-hygienists-should-never-treat-patients-with-active-oral-herpes/
- Medline Plus, U.S. National Library of Medicine, National Institutes of Health https://medlineplus.gov/herpessimplex.html
- Bowen DM (ed.) and Pieren JA (ed.). Darby and Walsh Dental Hygiene: Theory and Practice (5 th edition). St. Louis: Elsevier Saunders; 2020.
- Heymann D (ed.). Control of Communicable Disease Manual (20 th edition). Baltimore: American Public Health Association; 2015.
- Little JW, Falace DA, Miller CS and Rhodus NL. Dental Management of the Medically Compromised Patient (9 th edition). St. Louis: Elsevier Mosby; 2018.
- Ibsen OAC and Phelan JA. Oral Pathology For The Dental Hygienist (6 th edition). St. Louis: Saunders Elsevier; 2014.
- Regezi JA, Sciubba JJ, and Jordan RCK. Oral Pathology: Clinical Pathologic Correlations (6 th edition). St. Louis: Elsevier Saunders; 2012.
Cold Sores and the Dentist
On February 12, 2020 Written and Reviewed by JDC Content Committee

What is a Cold Sore?
Cold sores , also known as fever blisters, are caused by the herpes simplex virus type one (HSV-1). The virus lives in your nerves but damages your skin. It causes sores around the face, usually the lips, that last about one week. In rare cases, cold sores can appear on other parts of your body.
The virus spreads easily by coming in contact with the skin or bodily fluids of an individual with HSV-1. About two-thirds of people carry the HSV-1 infection, but some of them develop cold sores. The combination of a specific genetic component and a trigger (like fever, stress, or too much sun) leads to outbreaks.
Many people experience tingling, burning, or itching sensations prior to an outbreak. The site of the outbreak swells and reddens prior to the appearance of blisters. When the blisters pop, they form cold sores. Eventually, the sores will scab or crust over. Once the crust falls away, the sore is healed.
HSV-1 can be managed but not cured. Prescription antiviral creams can shorten limit the duration of an outbreak, and over-the-counter creams can help with the symptoms.
Though contagious, cold sores are not usually dangerous. However, there are some rare cases that necessitate a visit to a medical professional.
- Your cold sore lasts more than one week without crusting over.
- The cold sore interferes with your ability to speak or swallow.
- Your outbreak is accompanied by a fever.
- You experience a second outbreak of blisters.
What is a Canker Sore?
Canker sores appear on the inside of the mouth and they vary in size. Several factors, like an injury or stress, can cause a canker sore to appear. They vary in size and can occur on the gums, insides of the cheeks or lips, on the tongue, or the roof of the mouth.
It generally takes a week or two for canker sores to heal. Smaller canker sores usually go away on their own with minimal discomfort. Larger canker sores tend to be more painful and may be soothed by over-the-counter creams and gels or prescription treatments, like mouthwashes.
What is the Difference Between Cold Sores and Canker Sores?
Cold sores and canker sores are sometimes used interchangeably because they look and feel alike. However, canker sores and cold sores differ in a few notable ways.
- Cold sores are caused by HSV-1 while canker sores occur due to other conditions.
- The virus that causes cold sores is contagious, but canker sores are not.
- Cold sores appear on the face, usually around the mouth. Canker sores only occur inside the mouth.
Can I Go to the Dentist with a Cold Sore?
Should you go to the dentist with a cold sore? In most cases, no, you should cancel and reschedule your appointment. Since cold sores are caused by a highly contagious virus, there is a risk of spreading it to other people when you have an active outbreak.
It may seem far-fetched that a small sore on your upper lip could cause problems, but until that sore has scabbed and crusted over, the underlying virus is active. Even the most innocent exchange, like touching your mouth and then using a pen or doorknob could pass on the virus.
While you may be afraid to cancel, your dental team will appreciate your concern for their well-being. Contact the office and be honest about your reason for canceling. Keep in mind, cold sores usually last a week or two, so reschedule far enough out to give yourself time to heal.
If you have questions or concerns about cold sores, the team at Jefferson Dental Care can answer them. Contact the clinic nearest you to make an appointment. We’re here to help you keep your mouth healthy!
Our Jefferson Dental Content Committee supports our team by educational and informational articles related to what we do, oral care tips, and current events in our communities.
This blog provides general information and discussions about oral health and related subjects. The information and other content provided in this blog, website or in any linked materials are not intended and should not be considered, or used as a substitute for, dental advice, diagnosis or treatment. This blog does not constitute the practice of any medical, dental or other professional health care advice, diagnosis or treatment. We cannot diagnose conditions, provide second opinions or make specific treatment recommendations through this blog or website.
If you or any other person has an oral health concern, you should consult with your dentist or seek other professional dental treatment immediately. Never disregard professional medical/dental advice or delay in seeking it because of something that you have read on this blog, website or in any linked materials. If you are experiencing a dental emergency, please visit your local Jefferson Dental & Orthodontics office — we accept walk-ins.
Related Stories

Jefferson Dental Sponsors Traders Village
On January 5, 2013

“Jeffy” Motivates Local Kids to Keep Their Teeth Clean
On May 23, 2013

Don’t Wait Till It Hurts: Periodontal Disease
On June 20, 2013
Skip Navigation
Oral Health

Social Impact
Whitening Products
Whitening Solutions
- All Optic White® products
- Pro Series Toothpaste
- Overnight Teeth Whitening Pen
- Renewal Toothpaste
- Advanced Toothpaste
- Stain Fighter® Toothpaste
- Charcoal Toothpaste
- Whitening Mouthwash
Healthy Habits
- Brushing & Flossing
- Mouth & Teeth Anatomy
- Nutrition & Oral Health
- Selecting Dental Products
- Threats to Dental Health
- Teeth Whitening
Common Problems
- Gum Disease
- Mouth Sores & Infections
- Plaque & Tartar
- Temporomandibular Disorder (TMD)
- Tooth Sensitivity
Dental Conditions
- Adult Orthodontics
- Anorexia/Bulimia
- Bridges & Crowns
- Cleft/Lip Palette
- Dental Emergencies & Sports Safety
- Dental Visit
- Diabetes & Endocrine Disorders
- Gastrointestinal Disorders
- Heart Disease
- HIV/AIDS & STDS
- Immune Disorder
- Kidney Disease
- Respiratory Conditions
- Root Canals
- Tooth Removal
Life Stages
- Infant Oral Care
- Children's Oral Care
- Teen Oral Care
- Adult Oral Care
- Oral Care During Pregnancy
- Adults Age 55 and Up
- View all articles
- Manual Toothbrush
- Battery Toothbrush
- Whitening Kits
- Specialty Products
- Toothbrush with replaceable heads
- Cavity Prevention
- Enamel Protection
- Fresh Breath
- Plaque Prevention products
- Sensitive Relief
- Tartar Control
- Tooth Whitening
- Colgate ® Total ®
- Colgate ® Max White ®
- Colgate ® Kids ®
- Colgate ® Sensitive ®
- Colgate ® Sustainable Toothbrushes ®
- Colgate ® Max White Ultra ®
- Colgate ® Keep ®
- View all products
- For Parents
- For Teachers
- For Dental Professionals
- View all resources
- Giving Back
- Sustainability
- Accessible Oral Care
- Innovation Champions

Cold Sores and Fever Blisters: Causes & Remedies
Top articles, more articles.
Cold sores and fever blisters are caused by herpes simplex virus type 1 (HSV-1). This virus is passed from person to person by saliva (either directly, or by drinking from the same glass or cup) or by skin contact. Cold sores usually appear as clusters of tiny blisters on the lip. About 8 out of 10 people have the virus that causes cold sores. Most people are first infected before they are 10 years old.
After this first infection, the virus remains dormant (inactive) in the nerves of the face. In some people, the virus becomes active again from time to time. When this happens, cold sores appear. HSV-1 can get active again because of a cold or fever.
Stress also can lead to a cold sore outbreak. This includes mental and emotional stress, as well as dental treatment, illness, trauma to the lips or sun exposure. HSV-1 also can infect the eyes, the skin of the fingers and the genitals. Most genital herpes infections are caused by herpes simplex type 2 (HSV-2), however.
HSV-1 can cause serious illness in people who have other health problems. The virus also can cause serious illness in people whose immune systems are weakened by either illness or medicines they are taking.
People infected with HSV-1 for the first time may have fever, headache, nausea and vomiting. They may have painful swelling and open sores in the mouth. Some people have a sore throat. These symptoms usually begin about a week after someone is exposed to HSV-1.
Cold sores appear when HSV-1 is reactivated later in life. They may occur after a period of illness or stress, poor nutrition or sunlight exposure. Sometimes there's no known reason. Dental procedures that stretch the lip may occasionally trigger the virus.
The border of the lip is the most common place that these sores appear. They may occasionally occur inside the mouth, too. This is more likely in people who have weakened immune systems or other medical problems.
The first sign of a cold sore is a tingling, burning or itching. This is followed by swelling and redness. Within 24 to 48 hours, one or more tiny blisters ("fever blisters") appear. These blisters pop and form painful sores ("cold sores"). The sores eventually are covered by crusts, which look like scabs. The crusts are shed and form again while the sore heals.
Your dentist or physician usually can diagnose cold sores by asking you about your medical history and examining you. If you have other medical conditions, your physician may do other tests to diagnose cold sores. These tests are usually not necessary in healthy people.
Expected Duration
When you are first infected with HSV-1, symptoms can last for 7 to 14 days. Cold sores usually crust within 4 days and heal completely within 8 to 10 days.
To help to prevent a first herpes infection in children do not let them be kissed by anyone who has cold sores, fever blisters or signs of a first herpes infection. However, HSV-1 is very common. Most children will be infected by the time they reach adulthood. Several different vaccines are being developed against HSV (types 1 and 2), but these appear to protect only people who have never been infected.
There is evidence that using sunscreen on your lips will prevent cold sores caused by sun exposure. Antiviral medicines may prevent cold sores from forming. In certain situations, your dentist or physician may prescribe these medicines. If you expect to encounter a known trigger, a medicine taken in advance can decrease the chance of a cold sore.
Some medicines can help cold sores heal faster. They also relieve pain and discomfort. The medicines are acyclovir (Zovirax), famciclovir (Famvir) and valacyclovir (Valtrex). These drugs cannot get rid of the virus. You need to take them each time you can feel a cold sore coming on. Once you have blisters on your lip, the medicines will not help much.
These drugs also can stop cold sores from popping up in the first place. Some people take them when they know they will be under stress.
Keep the area clean and apply lip balm. Try not to touch the area. Do not pick at the crusts over the sores. Avoid kissing anyone while you have blisters and sores. Cold sores can spread through kissing and by sharing things that touch the lips and the skin around them, such as spoons, forks, glasses and towels.
When to Call a Professional
Cold sores are common. They usually are not dangerous. If you have a weakened immune system (because of a disease, or because of medicines you take), HSV-1 can cause a serious illness. Call your dentist or physician right away if:
- Lip or mouth sores persist longer than one week
- The sores make it hard for you to talk or swallow
- You develop a fever
- You have a second outbreak of blisters
HSV-1 infection is a lifelong problem.

Want more tips and offers sent directly to your inbox?
Sign up now
This article is intended to promote understanding of and knowledge about general oral health topics. It is not intended to be a substitute for professional advice, diagnosis or treatment. Always seek the advice of your dentist or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment.
Related Products
You might also like.

Submit an Idea
Modern Slavery Statement
WEEE & Battery information
United Kingdom (UK English)
Colgate Palmolive Pension Plan
ColgateProfessional.co.uk

© YYYY Colgate-Palmolive Company. All rights reserved.
Terms Of Use
Privacy Policy
All Products
Children's Privacy Policy
All Articles
Cookie Consent Tool
Cookie Policy

How To Prevent Cold Sores After Dental Work? (Ultimate Guide)
Have you noticed that every time you go to the dentist, cold sores would start showing up around your mouth? You might brush it off as pure coincidence, but there are actually several reasons why this happens often after getting dental work done.
Cold sores aren’t just embarrassing—these mouth ulcers are painful, too. If getting painful cold sores is a common occurrence for you after you visit the dentist, you might want to go the extra mile and prevent them from showing up.
Today, we’ll take you through how to prevent cold sores after dental work, along with why these blisters show up in the first place. We’ll also share our top tips for caring for these sores if you do end up with them after a trip to the dentist.
Why Do I Keep Getting Cold Sores After Visiting the Dentist?

Cold sores, sometimes referred to as fever blisters, are small, red, painful blisters that form around the lips and mouth. They’re caused by a specific herpes simplex virus type called HSV-1—a common kind of herpes that results in infections near the mouth.
Don’t panic—HSV-1 is far from the dreaded genital herpes. Most people will get HSV-1 early in their childhood, maybe even in infancy. That’s why kids often complain about sores when they have them. It is transmitted through saliva or skin-to-skin contact , making it highly contagious.
After you initially catch this virus, it doesn’t go away. It just stays in your body in a dormant state until adulthood. When you have a weak immune system or get stressed , the virus comes alive again, which leads to cold sore outbreaks.
Other symptoms of cold sores from HSV-1 include itching in the mouth area, sore throat, fever, swollen lymph nodes, and feeling like your mouth is drier than usual.
But why do cold sores appear after getting dental work done? The answer is simple—trauma to the mouth.
When you’re in the dentist’s chair getting your teeth done, you might experience trauma to the lips. Small wounds or irritation to the mouth area weaken the tissues there, making it easy for a dormant HSV-1 to reactivate. As a result, you’ll see a fluid-filled blister or two near your mouth.
If you haven’t been infected with HSV-1 before, then you might have gotten the virus from the dental office. The dental clinic, after all, is a healthcare setting where diseases can be transmitted unknowingly.
Tips to Prevent Cold Sores After Dental Work

Want to ensure that you won’t experience those dreaded cold sores and scabs after your trip to the dentist this time around? Here are some ways you can prevent them from popping up around your lips and mouth.
1. Have a strong immune system before your appointment
Whether you haven’t gotten HSV-1 before or have a dormant virus in your body, making sure your body is strong and healthy keeps outbreaks at bay if you catch the virus. A weakened immune system will make you more susceptible to developing cold sores.
So, make sure that when you book your dental appointment, your body feels at its best. If you have a fever or severe headache on the day of your appointment, it might make you more vulnerable to cold sores later on. It might be best to delay your scheduled procedure until you’re better.
To ensure that your immune system is fine before getting dental work done, get a lot of rest and don’t fall victim to stress, as it’s a common trigger of HSV-1 cold sore outbreaks . Eat healthy food and make sure to take your daily dose of vitamin C in the days leading up to your appointment.
2. Ask your doctor for antiviral medicines
Speak with your trusted doctor to tell them about your cold sore situation that happens every time you visit the dentist. Ask them if there are any prescription antiviral medications you can take before going to the dentist to keep it from happening again.
3. Maintain excellent oral hygiene
A clean mouth is a healthy mouth. So, before your appointment, practice the best oral hygiene you can. Always brush your teeth, floss, and gargle with mouthwash to get rid of any bacteria that can make its way to your lips, aggravating any virus.
4. Practice proper lip care to avoid trauma to the lips
Before heading to the dentist, make sure your lips are healthy and moisturized. If your lips are dry, they are more likely to crack while the dentist works on your teeth. As a result, your skin can break, allowing viruses and other bacteria to enter. This can lead to cold sore outbreaks.
You’ll also want to avoid picking at the skin on your lips in the days leading up to your appointment. Any wound or lesion you accidentally cause while doing so can make you vulnerable to cold sores.
If you can, use an SPF-infused lip balm regularly. Not only will this moisturize your lips, but it can also protect them from excess sun exposure—another trigger of cold sores.
What to Do If You Get Cold Sores Anyway

If you still end up getting cold sores after your dental appointment, don’t worry. The best cure for cold sores is to allow the natural healing process to take place. In about 7-10 days, your cold sores will heal completely—as long as you don’t pick at them or try to “pop” the blisters, of course.
Here are some things you should consider doing while you’re nursing your cold sores:
- Keep your lips and mouth area clean. Wash the area with a gentle cleanser or a saline solution to keep the sores from getting infected.
- Use a topical ointment like Zovirax, Valacyclovir, or Acyclovir to treat the blisters and help them calm down. Not only will your sores feel less painful afterward, but this cream can also speed up their healing process.
- Put a cold compress on your blisters, especially when they look and feel inflamed. This can help soothe the pulsating pain from the cold sores.
- If your sores are painful, you can manage the pain at home with over-the-counter pain relievers. For kids in particular, check with your family doctor about what medications they can take to keep the pain of cold sores at bay.
- Avoid hot and spicy foods. Sparkling beverages and acidic, citrusy fruits should also be avoided until the sores get better. These can be irritating to open blisters and can make the pain worse. They may also lead to an infection.
- Practice good hygiene at home. Remember, HSV-1 is highly contagious. Don’t share utensils, glasses, and even towels with other people, lest you pass on the virus to them. Avoid kissing and hugging others to limit the transmission of the virus.
If You Have Cold Sores Before Visiting Your Dentist…
If you have cold sores before your appointment, is it still a good idea to push through with it? Maybe not, but only your dentist will be able to give you sound advice on your situation.
All you have to do is be transparent. Call up your dentist before your schedule and notify them that you’ve noticed some blisters around your mouth. They’ll help you assess your cold sores. If you find that the sores are in their active stage, you will likely be asked to reschedule your dental work.
Dental clinics need to be as safe and sterile as possible to keep every healthcare worker and patient safe and healthy. If you have an active cold sore outbreak, you may compromise the clean, virus-free environment of the dental clinic and pass on the virus to people there.
Plus, if you end up getting your dental work done even with cold sores, there’s a good chance they’ll be even more painful from you opening your mouth a certain way. And if the blister is accidentally punctured, the infection can spread to other areas of your face, like your cheek.
Still not sure if you should book an appointment with your dentist if you have cold sores? Check out what this dentist has to say about the matter so you can weigh the risks before choosing to come in for dental work:
For some people, cold sores are a normal part of getting dental work done. But it doesn’t mean you should just tolerate or be a slave to them. Instead, follow the preventive measures and precautions we listed above to keep them at bay even after a long trip to the dentist’s office.
If you still end up getting cold sores, don’t worry. They will likely clear up in a few days. Just try to keep the area clean and avoid foods that will irritate it.
The best way to avoid getting cold sores altogether after visiting the dentist is to make sure you’re strong and healthy before even booking an appointment. Keep these measures in mind next time you’re anxious about going to the dentist and getting sores again. Your lips will thank you.
Related posts:
- What Is Dental Gold? (Ultimate Guide)
- How Much Does A Dental Check Up Cost? (Ultimate Guide)
- How Many Dental X-rays Are Safe In A Year? (Ultimate Guide)
- How Much Do Dental Crowns Cost? (Your Ultimate Guide)
- What Is A Dental Deep Cleaning? (Ultimate Guide)
- How Much Does A Dental Visit Cost? (Ultimate Guide)
- What Does Restorative Dental Treatment Cover? (Ultimate Guide)
- How Much Does A Dental Filling Cost? (Ultimate Guide)
Similar Posts

Can teeth with holes be saved? (tooth decay process & treatments)
Tooth decay leading to cavities is an extremely prevalent problem affecting people of all ages. Cavities develop…

Can Bottom Teeth Be Built Up? (Step-By-Step Process)
Your teeth endure a lot over your lifetime. The daily wear and tear of biting and chewing…

What To Eat After Dental Surgery? (84 Excellent Suggestions & Other Tips)
Going through oral surgery is rarely fun but the recovery time afterward can be equally annoying. There…

3 Steps to Get Dental Implants Covered by Insurance
If you’ve lost a tooth or need to have one extracted, you’ll probably be thinking about your…

Can you file down big teeth?
Overview of filing down teeth Filing down teeth, also known as enamel shaping, is a procedure that…

Can you see teeth in baby gums? What’s the sign?
When do babies’ teeth start coming in? Most babies get their first tooth between 6 and 10…

Canker Sore After Dentist Visit: Why & How To Treat Properly!
Canker sores after dental treatment
Which dental work causes mouth sores.
Aphthous ulcers, also known as canker sores, are a common oral health problem. They appear as round, yellowish or whitish ulcers on the mouth’s lips, cheeks, tongue, and floor. They are often painful and can be single or multiple. Although they are not dangerous and do not cause a fever, they can irritate and make you uncomfortable. If your child develops aphthous ulcers, there is no need to worry – is it possible that you can get one after visiting a dentist?
Canker sores are a common problem that can occur after dental treatment. They are small, painful ulcers that can make it difficult to eat or speak. While there is no cure for canker sores , there are steps that you can take to help reduce their severity and shorten the duration of the outbreak.
If you experience canker sores after dental treatment, here are a few things that you can do to help relieve the pain and speed healing:
- Apply ice or a cold pack to the sore for 10-15 minutes daily. This will help reduce inflammation and pain.
- Take over-the-counter pain medications such as ibuprofen or acetaminophen to help relieve pain.
- Rinse your mouth with salt water several times a day to help keep the area clean and help promote healing.
- Avoid eating acidic or spicy foods, as these can aggravate the sore and prolong the healing process.
- If necessary, you may also want to consider taking an over-the-counter oral steroid medication to help reduce inflammation and speed healing.
If you experience canker sores after dental treatment, there are a few things that you can do to help reduce their severity and shorten the duration of the outbreak. Following these tips can help keep your mouth healthy and pain-free.
Is it common to get a canker sore after dental work?
Canker sores are a common problem that can occur after dental treatment. They are small, painful ulcers that can make it difficult to eat or speak. While there is no cure for canker sores, there are steps that you can take to help reduce their severity and shorten the duration of the outbreak.

Any dental work can potentially cause canker sores.
Common triggers include:
- tooth extractions
- dental cleaning
- dental injection (novocaine shot)
- wisdom tooth removal
If you have a canker sore, you may notice a tingling or burning sensation a day or two before the sore appears. The sore is usually round or oval and white or yellow with a red border. Canker sores typically heal within two to three weeks without treatment. However, they can be painful and make it difficult to eat or drink.

How To Fix Receding Gums At Home & Other Possible Treatments!


Should You Floss Teeth Twice A Day? Can You Floss Too Much?

Stabilizing Smiles: A Comprehensive Guide to Treating Loose Teeth

Navigating Dental Accidents: A Comprehensive Guide to Prevention, Emergency Response, and Recovery

Mouth Sores from Chemo: Causes, Prevention, and Treatment

What Does a Canker Sore Look Like? Identifying Symptoms and Treatment Options
Privacy Policy
- Orthodontics Niche Guest Post Offer: Write for Us and Share Your Expertise
- Write for Us in the Dentistry Niche: Guest Post Offer

Compare items
- Total ( 0 )
Understanding Flu-like Symptoms After Dental Work
Is feeling sick after the dentist normal.
- While most people do not have any adverse reactions to dental work, some may experience flu-like symptoms after a visit to the dentist. These symptoms can include a fever, chills, fatigue, and aches and pains throughout the body. While it is not common, it is vital to be aware of the potential side effects of dental work so you can take the necessary steps to alleviate any discomfort or symptoms that may arise. If you experience these symptoms after a visit to the dentist, be sure to contact your healthcare provider to determine the cause and the best course of action.
Common Symptoms After Dental Treatments
- After a dental procedure, you may experience symptoms such as nausea, jaw soreness, and a sore throat. Nausea can be caused by the numbing agent used during the procedure. Soreness in the jaw and lip area may be due to using dental tools during the procedure. Ear pain, pressure, and extreme pain are also common symptoms. Additionally, a sore throat may develop from an open mouth during the procedure. If these symptoms do occur following dental treatments, they typically last a few days.
Factors Contributing to Flu-like Symptoms After Dental Work
- A weak immune system or underlying health conditions may contribute to developing flu-like symptoms after dental work. Taking certain medications may also impact your immune system. Due to weakened immune systems, individuals undergoing chemotherapy or radiation treatment may be more susceptible to flu-like symptoms. Additionally, individuals with autoimmune diseases, such as lupus, or conditions, such as diabetes, are more likely to experience symptoms. Following a healthy lifestyle before and after treatment is your best option to prevent these symptoms.
How to Prevent Flu-like Symptoms
- Preparation is key when it comes to preventing flu-like symptoms after dental work. By maintaining healthy habits such as eating healthy, limiting sugar and alcohol intake, exercising, and taking vitamins, you can help boost your immune system and reduce the likelihood of developing flu-like symptoms. Regular check-ups with your dentist and primary care physician can also help detect underlying health conditions that may impact your overall health.
Seek Professional Guidance if You Experience Symptoms
- If you start to experience flu-like symptoms after dental work, it is imperative to consult with your dental team. Your team can help diagnose and treat the symptoms. Treatment options may include over-the-counter pain medications, prescribed medication, or recommendations for alternative remedies. Additionally, asking questions and being proactive with your healthcare team can help prevent future occurrences of flu-like symptoms after treatments. Flu-like symptoms after dental treatments are common and can indicate underlying health issues. One can take preventative measures to avoid these symptoms by living a healthy lifestyle, maintaining routine dental visits, and staying on top of their overall health. Communicating with your dental team if you experience flu-like symptoms after treatments is essential, as your providers can adjust or provide further treatment. By prioritizing your health, you can maintain a healthy smile and an overall healthy lifestyle. Contact St. George Dental Care today with any further questions to schedule a consultation with our premier dentists.
Contact St. George Dental Care Today
Check out what others are saying about our services on Yelp: Read our Yelp reviews .
Recent Posts
Unlocking the secrets of resin veneers: enhancing your smile.
Are you tired of feeling self-conscious about your teeth every time you smile? Do imperfections such as discoloration or uneven spacing make you hesitant to show off your pearly whites? Say goodbye to these insecurities with the help of resin veneers. This revolutionary cosmetic dentistry solution has become increasingly popular in recent years, providing individuals…
Say Goodbye To Tooth Sensitivity After Dental Cleanings
Welcome to our dental blog, where we strive to provide valuable information about oral health and hygiene. If you dread going to the dentist because of the pain and discomfort caused by tooth sensitivity after cleanings, this post is for you! Sensitive teeth can significantly impact your quality of life, making it difficult to enjoy…
How To Assess And Repair Damaged Dental Crowns
Dental crowns, otherwise known as dental caps, are an essential aspect of modern dentistry and are typically used for restorative and cosmetic purposes. They are designed to restore the shape and function of a damaged, decayed, or broken tooth while improving its overall appearance. In this blog post, we'll discuss the various types of crown…
Bye-Bye Hard Tooth Plaque: Say Hello To A Healthier Smile!
Get ready to say goodbye to stubborn tooth plaque and say hello to a brighter, healthier smile! St. George Dental Care proudly presents the ultimate guide on combating hard tooth plaque. As we all know, oral health is crucial for our overall well-being and is a reflection of our internal health. While brushing twice daily…

- Privacy Policy
Book Your Appointment Today!
- Activate Black Text
- Activate White Text
- Increase Font Size
- Decrease Font Size
- Reset Accessibility Options
- Chinese (Simplified)
- Living Well Daily
- Free Articles
- Meet Dr. Scott Olson, ND

Caution: Dental Work Can Cause Herpes Outbreaks
- Find out more about the hidden dangers at your dentist office
- If you’ve ever had a cold sore, you NEED to read this
- Two supplements to help you claim victory over viruses.
Dear Living Well Daily ,
A while back, my friend underwent a dental extraction. A few days after, she asked me to pick up a prescription for her and bring it over. I quickly agreed, but before I hung up, she threw out a brief disclaimer, “ Don’t judge me for this prescription or what I look like. I caught something nasty at the dentist. ”
I didn’t think much of her warning. I just assumed she was surprised by the strength of the pain pills she was prescribed and perhaps had an infection from her procedure.
But when I got the script, I must admit, while there was no judgement, I was a bit confused. You see, the drugs she had me pick up were for a viral infection that had little to do with oral surgery (or at least that’s what I thought at the time).
But when I saw her, I was truly shocked . My friend had painful lesions all over her lips and lower face. She was having a hard time speaking and was visibly uncomfortable. And when she told me what happened, my mind was blown…
My friend was suffering from a major oral herpes outbreak.
And it seemed that her dental work was the catalyst for the torturous state she was in, even though her dentist had taken precautions to protect her.
Like many folks, she had a history of cold sores (three in her lifetime, to be exact). Nothing major, every handful of years a tiny bump would pop up on her upper lip and disappear a few days later. Because of this, her dentist put her on antiviral medications before her procedure to try to prevent an outbreak.
You see, cold sores are caused by herpes simplex virus type 1 (HSV-1), a common viral infection. In fact, According to the National Institutes of Health, HSV-1 is so run-of-the-mill that about 90 percent of American adults are exposed to the virus by the age of 50. Before an outbreak, itching, burning and tingling sensations are common symptoms. During the outbreak, painful fluid-filled blisters occur and then eventually scab or crust over before they heal.
And while there are treatments to control herpes, there is no cure. The virus can lie dormant in the nerve tissue of the face. When the virus is reactivated, it can cause outbreaks.
Despite it’s prevalence, many people never experience symptoms or outbreaks. However, this means they could infect others unwittingly, or experience an unexpected outbreak following a trauma like dental work.
Unfortunately for my friend, the precautionary course of antivirals she took before the procedure did her no good — she still suffered a serious outbreak. You see, studies show that having intense dental work such as an extraction can trigger severe herpes outbreaks. It’s unclear whether the extraction itself or anesthesia, or both are to blame for the outbreak. While anyone with the virus could be susceptible to a post dental flare-up, it’s more likely to happen to folks who experience cold sores.
Therefore, she didn’t actually catch herpes from the dentist, but rather suffered a nightmarish outbreak triggered by her procedure.
After another course of antivirals, her blisters healed. She hasn’t had an outbreak since. The experience was so traumatic, though, she carries antivirals everywhere she goes, just in case she feels an outbreak coming on.
But it seems she isn’t alone. Just surf the net a bit and you’ll find other cases of these types of trauma-induced outbreaks — everything from dental work to lip injections, and tattooed make-up can ignite a surprise onset.
However, there are ways to protect yourself and a few antiviral supplements that may help you lower your risks of outbreak.
First things first here. The best way to avoid a herpes outbreak is to not catch the virus. However, as we mentioned earlier, this is not an easy thing to do. However, there are a few things you can do to lessen the risk:
- Avoid intimate contact with anyone who’s showing signs of infection (i.e., cold sores, fever blisters). While you can still catch the virus from someone who doesn’t have immediate symptoms, it’s more likely to happen during an outbreak
- Never share razors, towels, dishes or other items that may have come in contact with an open herpes sore
- If you’ve ever had a cold sore, be sure to report it to your dentist or doctor before any oral medical procedure. This way your practitioner can take the proper steps to try to avoid a trauma-induced outbreak. You can also request that your practitioner prescribe antiviral medications prior to your procedure steps if you’re concerned about a potential outbreak, even if you’ve never had symptoms.
Recently, a study in the Journal of Pineal Research shows that some natural antivirals are as strong as prescriptions. Acyclovir, a common antiviral prescribed for herpes (and the one my friend was taking), was compared to a natural compound that contained melatonin, phosphate, magnesium and fatty acids in the treatment of oral herpes.
At the completion of the study, researchers found that the natural treatment group experienced a 95 percent rate of complete regression of symptoms in seven days. The prescription group, however, saw an 85 percent rate of complete regression in seven days. This means that while both treatments worked, the natural compound was slightly more effective.
The exact doses for this compound are unavailable, or we would share them with you. However, it is noted that it contains 2.5 mg of melatonin. It would make sense that supplementing with melatonin may be one way to help you manage oral herpes, as it is a powerful antioxidant. Not to mention it’s an effective sleep aid!
Another effective natural antiviral is St. John’s wort because it contains hypericin. Hypericin is a chemical that can penetrate nerve cells and destroy the fatty coatings on the virus, killing it off. According to the Weston A. Price Foundation, taking two 1.8 gram tablets a day long term can help curtail outbreaks. Click here to check it out.

Natalie Moore Managing editor, Living Well Daily
[1] Mouth Infections
[2] Severe herpes simplex virus type-I infections after dental procedures.
[3] Risk of Transmission of Viruses in the Dental Office
[4] The Weston A. Price Foundation: Herpes
[5] Effect of black tea extract on herpes simplex virus-1 infection of cultured cells
Written By Natalie Moore
Natalie Moore is a dedicated health researcher with a passion for finding healthy, natural, and science-based solutions. After a decade of direct healthcare experience in western and natural medicine, she was involved in public health research before joining Living Well Daily.
View More By Natalie Moore
View More Free Articles
Belly Trick BOOSTS Brain Function
By Dr. Scott Olson, ND Posted April 14, 2024
Boy do I love a cheap and easy solution. And if you can’t resist a good bargain either, keep reading. Because I have a brain-boosting one to share that fits the bill. If you’re like most folks, you intend to stay as sharp as a tack well into your golden years. So, you’re always on...

The Hidden Heart Danger LURKING in Your Gut?
By Dr. Scott Olson, ND Posted April 13, 2024
Dear Living Well Daily Reader, Living with inflammatory bowel disease (IBD) is no walk in the park. The cramping, the urgency, the endless trips to the bathroom—it’s a daily struggle that can leave you exhausted and frustrated. And here’s the kicker: sometimes, IBD’s vague symptoms can lead to misdiagnosis or even NO diagnosis at all....

Has the Key to Unlocking Better MS Treatments Been Found?
By Dr. Scott Olson, ND Posted April 12, 2024
Dear Living Well Daily Reader, Imagine waking up one morning and feeling a strange tingling in your fingers. You brush it off, thinking it’s just a pinched nerve. But then, your vision starts to blur, and your balance is thrown off. Suddenly, you’re faced with a terrifying reality: you have multiple sclerosis (MS). For the...

6 Secret Ways to Spot HIDDEN Processed Foods
By Dr. Scott Olson, ND Posted April 11, 2024
“Avoid eating processed foods,”—If I’ve said it once, I’ve said it a thousand times. The reason why is simple. These Frankenfoods are designed to satisfy your taste buds. But they leave your body full of foreign chemicals that can cause harm and in need of more nutrients. But a patient asked me the other day,...

8 Red Flags There’s a Heart Attack in YOUR Future
By Dr. Scott Olson, ND Posted April 10, 2024
Humor me and count to 40. Done? According to the Centers for Disease Control and Prevention (CDC), someone in the United States just had a heart attack. That adds up to around 805,000 people a year. Many of those were a “silent” heart attack, with the victim having no clue it even happened—and they go...

Mailbag! Neuropathy Pain? Ease Tingling in Hands and Feet
By Dr. Scott Olson, ND Posted April 9, 2024
“I’m diabetic and have burning, tingling pain in my feet. My doctor says it is peripheral neuropathy, and there aren’t any cures. But do you have any tips to help me deal with it?” —Hank Hi Hank, Uncontrolled blood sugar can trigger nerve pain called peripheral neuropathy. This condition causes pain and numbness, usually in...

5 Often Overlooked Diabetes Red Flags
By Dr. Scott Olson, ND Posted April 8, 2024
Some of the worst diseases we face are also the stealthiest. They silently sneak up with few signs that they’re harming us from the inside. Well, that is until it’s too late, and they’re well-established. Osteoporosis and hypertension are on that list. And so is type 2 diabetes. In fact, scientists estimate that around 25...
ALERT: CGMs Can Give Inaccurate Glucose Readings
By Dr. Scott Olson, ND Posted April 7, 2024
Keeping your blood sugar in check is critical for a longer, healthier life. It used to be if you wanted to watch your blood sugar for hours at a time, you’d have to go to a lab and be hooked up to an expensive, complicated machine. But now, anyone can get a continuous glucose monitor...

“Eat the Rainbow” Trick Drives Down Cancer Risk
By Dr. Scott Olson, ND Posted April 6, 2024
If I were to ask you, “What’s the color of good health?” what would you say? Maybe it’s green or blue, the “colors of nature.” Or rosy pink cheeks may come to mind. Well, it turns out the “colors of the rainbow” might be the best answer. Research suggests the key to a long, healthy...

Unexpected Danger LURKS in Your Drinking Glass
By Dr. Scott Olson, ND Posted April 5, 2024
I’ve said it so often I’m in danger of sounding like a broken record. (For those folks old enough to remember them.) But this habit is such a threat to your health it’s STILL worth the risk. One of the WORST things you can swallow is sweetened beverages—made with natural and fake sugars. They’ve already...
Phone: (229) 377-6125 |
240 S Broad St, Cairo, GA 39828

Fever Blisters After Treatment

These multiple sores are the result of an oral herpes virus (herpes type 1 virus) that has been activated in the mouth of your child. The oral herpes virus can be activated by a number of factors including stress, chemical or physical insult, food or liquid sensitivity, or change in their immune response. The stress of dental treatment can, therefore, activate the virus. The virus is present in about 90 percent of children under age ten. Once it occurs as a primary attack, the child starts to develop immunity towards future attacks. However, it can reoccur as a mild attack around the lips in a significant number of children and adults when the virus is reactivated by such things as trauma, sunburn, stress, dental treatment, etc.
For the initial outbreak and infection, the duration of the illness is usually two weeks. Signs and symptoms of the viral infection typically occur within the first week and improve in the second week. As this is a contagious disease, it is recommended that the child be kept at home with limited exposure to others.
Over-the-counter, aspirin-free pain and fever relief medications should be used according to product label directions. Over-the-counter topical paste such as Orabase-b or Zilactin can be applied to the ulcers around the lips two to four times per day with a cotton swab. Toothpaste and brushing might be very painful, so use disposable gauze or Toothettes to carefully wipe the teeth and mouth.
Children should be encouraged to drink bland liquids such as water, carbonated liquids, etc., as often as possible to keep hydrated. Avoid the use of salty, spicy, acidic, and hot liquids or foods.
All people should avoid contact with the sores. All utensils, cups, plates, etc., used by the child should not be shared and should be washed in extremely hot water with detergent after each use.
For recurring lip sores, the blisters quickly form unsightly scabs and usually heal within one week. Over-the-counter topical anesthetics may help. Definitive control of the blister outbreak is limited to topical antiviral medications that provide temporary relief from discomfort but will not speed up the healing process. Currently there is no cure for recurrence of this viral infection. However, it is thought that antiviral therapy reduces the degree and severity of the outbreaks.
Office Hours
Mon & Tue: 8am-12pm & 2pm-5pm Wed & Thu: 8am-1pm & 2pm-5pm Fri – Sun: Closed
Appointments
We will do our best to accommodate your busy schedule. Please schedule an appointment today!
Request Appointment
Our Location

Financial Aid Available for Eligible Programs. Registration Now Open.
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
- Skip to footer
- 732-440-4110
ACI Medical & Dental School
A New Beginning, We Change Lives
" * " indicates required fields
Related Posts
- Tips for Stay at Home Moms Going Back to School
- Becoming a Physician’s Assistant in NJ? ACI Can Help!
- Earn Brookdale Medical Terminology Credits at ACI
- The Benefits of Dual Certification at ACI
- Tick Season in New Jersey
Our Results Speak for Themselves
ACI Medical & Dental School students routinely exceed the rigorous standards required by the MSA (Middle States Association of Colleges & Schools).
- 93% Pass Rate on National Credential Exams (7/1/22 – 6/30/23)
- 91% Employment Rate (7/1/22 – 6/30/23)
- 60% COVID Graduation Rate * (IPEDS 9/1/19 – 8/31/20)
- 94% Prior Year Graduation Rate (IPEDS 9/1/18 – 8/31/19)
- *Due to the global pandemic, this cohort was unable to complete the full program, including internship, to meet the 150% regulation. The requirement of completing the program within 150% was not feasible during the onset of Covid-19.
Accredited By:

Credentialing By:

Approved By:

Contact ACI Medical & Dental School
Contact us today for more information about finding the program that is right for you and enrolling at ACI Medical & Dental School.
ACI Medical & Dental School
- 215 Broad Street Eatontown, NJ 07724
GI Bill® is a registered trademark of the U.S. Department of Veterans Affairs (VA). More information about education benefits offered by VA is available at the official U.S. government Web site at https://www.benefits.va.gov/gibill .
- Testimonials
- Meet Our Staff
- Graduations
- Medical Assistant Certification Program
- Dental Assistant Training Program
- Medical and Dental Administrative Assistant Program
- Secondary Programs
- VA Training Programs
- Federal Direct Loans
- Net Price Calculator
- Program Statistics
- Clery Act Policies
- Campus Crime Statistics
- Accreditation
- Information for High School Seniors
- Why Invest in Education?
- Convenient Programs
- Career Assistance Program
- Employment Opportunities
- In Demand Careers
- Hire Our Graduates
- Why Choose Legacy Dental
- Meet Our Doctors
- Meet The Team
- Our Technology
- Testimonials
- Smile Gallery
- Membership Plan
- Patient Forms
- Payment Portal
- Dental Crowns
- Porcelain Veneers
- Teeth Whitening
- Smile Makeover
- Dental Implants
- Partial Dentures
- Implant-Retained Dentures
- All on 4 Dental Implants
- Root Canals
- Dental Checkups
- Dental Cleaning
- Family Dentistry
- Tooth Extraction
- Dental Fillings
- Sedation Dentistry
- Wisdom Tooth Extraction
- Broken Dentures
- Mouth Sores
- Temporary Crown
- I NEED A CHECKUP AND CLEANING
- I WANT TO ENHANCE MY SMILE
- I HAVE ONE OR MORE MISSING TEETH
- I AM SCARED OF THE DENTIST
- I AM IN PAIN AND NEED HELP
- I WANT TO GET RID OF CAVITY IN MY TOOTH
- I have headaches or jaw pain
- I have crooked or crowded teeth
- I have bleeding or sore gums
- I don't have dental insurance
- I don't know exactly what I need

How to Treat Cold Sores with Laser Therapy (And Prevent Outbreaks)
Imagine this scenario:
You wake to a tingling, burning sensation on your lower lip and then remember the upcoming (insert important event here) you have this week… Dread and disappoint follow. If you suffer from cold sores, this narrative is all too familiar.
But don’t fret. Our dentists in Salt Lake City have some news to share with you on how to treat and prevent cold sores.
In this blog, we will discuss:
- How to tell if you have a cold sore
- How to prevent cold sores
- How to treat cold sores (spoiler alert – lasers!)
- How to know if you have a cold sore
A cold sore, also known as herpes labialis or a fever blister, is a harmless but irritating fluid-filled blister that goes away in about 10 days from the first symptom (tingling or burning sensation). They appear on the lips and sometimes the skin around the lips.
Herpes labialis, a cold sore virus, is contracted like any other virus. Usually, a person with an active fluid-filled blister exposes a person without the virus. An example of this would be a mother with an active cold sore kissing her child. When first infected, the symptoms mimic the common cold. The virus then can lay dormant in the body until it returns, presenting as sores on the lips.
Canker sore vs. cold sore
Often, cold sores are misidentified as canker sores. A canker sore is a white, yellow, or gray ulcer that occurs inside the mouth. Canker sores are usually caused by trauma (eg., chip to the roof of the mouth) or exposure to certain foods (e.g., citrus juices).
The best way to tell which one you have is, canker sores are inside the mouth, and cold sores are generally outside the mouth.
- What can you do to prevent cold sores?
So, you’ve got the virus already. What can you do to prevent future cold sore outbreaks? Many stimuli can put you at risk for a cold sore outbreak.
Risk factors that can cause an outbreak of cold sores are:
- Wind exposure
- Sun exposure
- Change in weather
Many of these risk factors are difficult to control, particularly stress. For tips on reducing stress, check out our blog post on stress and oral health .
Sun exposure is a big cold sore trigger, so be sure to use protection (sunscreen, hats, etc.) when in the sun to avoid a cold sore outbreak.
- Don’t cause a cold sore reinfection
If you already have an active cold sore blister, take care not to touch it. If you have touched the blister, wash your hands thoroughly. The fluid from the blister can spread and cause other blisters on noninfected areas of the lips, eyes, or fingers.
- How can you treat a cold sore?
For many, the option of waiting 10 days for a cold sore to heal is daunting or simply not possible. Although nothing will take away the cold sore instantly, many remedies help the blister go through the healing process faster.
The most common method to treat cold-sores has been ointments and oral medications, which are antivirals. A newer therapy is treating the sore with a laser.
- Laser therapy
At Legacy Dental , we provide laser therapy on active cold sores. This is best done in the tingling, burning stage of a cold sore. By catching it early, it will help the blister move through the healing phases faster and possibly make it not as big.
Laser therapy is a great cold sore treatment without side effects.
- What to expect with laser therapy
Getting a cold sore lasered is a quick, painless appointment. Our Salt Lake City dentists do not require an appointment for laser treatment of cold sores , and all of our doctors and hygienists are trained in treating cold sores.
After consultation between you and the dentist, you will be given safety glasses to wear. The laser will be used to treat the affected area. It is painless, and most people describe the sensation as feeling nothing or warmth. That’s it!
If cold sores are a recurring ailment for you or your case is extreme, our dentists may suggest medications.
- Now you know: How to avoid and treat cold sores with laser therapy
You can also refer back to this quick infographic outlining what you need to do to prevent and treat cold sores.
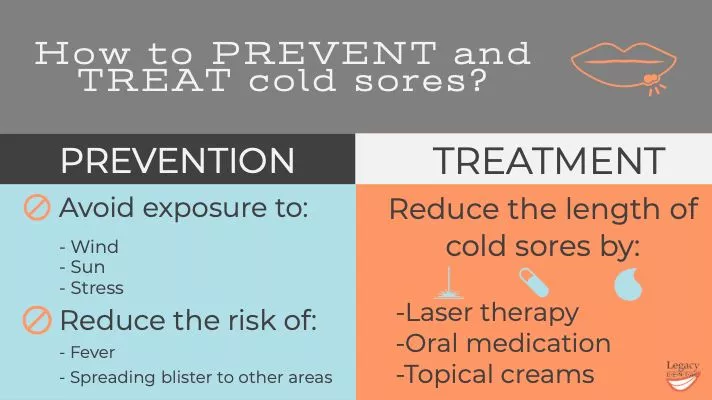
The next time you feel that telltale sign of a cold sore, don’t wait! Call us to treat your cold sore with laser therapy.
If you’re not currently experiencing a cold sore flareup, save our phone number , just in case!
Legacy Dental blog is proudly run by our Salt Lake City dentists team; We share knowledge about general dental care and practices. Apart from running this blog, we offer various dental services such as general dentistry, emergency dentistry , and dental implants for the community in Salt Lake City, Utah
How to reach us in and around Salt Lake City, Utah
Our Doctors Our Services New Patients Smile Gallery Blog Contact Us
South Salt Lake City Millcreek Holladay Murray Wildwood Zions Park
All rights reserved, Copyright 2024 Legacy Dental | Privacy policy | Sitemap Dental Marketing by WEB MARKETING FOR DENTISTS
" * " indicates required fields

Uncovering the Truth: Post-Dental Work Canker Sores Explained

1. Introduction: Understanding the Mystery of Post-Dental Work Canker Sores
Have you ever experienced the frustration of developing canker sores after dental work? We understand how painful and bothersome these sores can be, which is why we are here to shed some light on this mystery. In this post, we will explore the causes behind post-dental work canker sores and provide you with useful tips on how to prevent and manage them.
The Causes:
Canker sores, also known as aphthous ulcers, are shallow, painful lesions that can form inside your mouth. While the exact cause of post-dental work canker sores may vary from person to person, several factors can contribute to their development. Here are some common causes:
- Trauma: Dental procedures can cause minor injury or irritation to the delicate tissues in your mouth, leading to the formation of canker sores.
- Bacterial infections: Occasionally, various bacteria present in the oral cavity can invade the damaged tissue, increasing the risk of canker sore development.
- Allergies or chemical irritants: Some individuals may have a sensitivity or allergic reaction to certain dental materials, such as metals or acrylics, which can trigger canker sores.
By understanding these potential causes, you can take proactive steps to prevent post-dental work canker sores. Stay tuned for our next section, where we will dive deeper into effective prevention and management strategies!

2. The Basics: What are Canker Sores and Why Do They Occur after Dental Procedures?
Canker sores, also known as aphthous ulcers, are small and painful sores that can develop inside your mouth. They can occur on the inside of your lips, cheeks, tongue, or throat. These sores are typically round or oval in shape, with a white or yellowish center and a red border.
Canker sores can appear after certain dental procedures, such as orthodontic treatment or a dental cleaning. While the exact cause of canker sores is unclear, several factors can contribute to their development. These include:
- Accidental trauma to the tissues during the dental procedure
- Chemical irritants present in dental products or medications used during the procedure
- Stress or anxiety related to the dental visit, which may weaken the immune system and increase susceptibility to canker sores
If you experience canker sores after a dental procedure, it’s essential to maintain good oral hygiene to promote faster healing. Be sure to keep the affected area clean by gently brushing with a soft-bristled toothbrush and a mild toothpaste. Avoid any harsh or alcohol-based mouthwashes that can irritate the sores. Instead, rinse your mouth with a saltwater solution or an antimicrobial mouthwash recommended by your dentist.
3. The Role of Dental Work: Unveiling the Connection between Procedures and Canker Sore Formation
Are you someone who frequently develops canker sores after dental procedures? You’re not alone! Many individuals experience this frustrating phenomenon and wonder why it happens. Today, we’re here to shed some light on the connection between dental work and canker sore formation, helping you understand why these sores can sometimes appear after visits to the dentist.
1. Minor Trauma: Dental procedures, especially those involving extensive drilling or scraping, can cause minor trauma to the mouth tissues. Although the dentist’s goal is to minimize any potential damage, it’s common for these procedures to result in tiny cuts or abrasions. These small injuries are often the perfect entry point for a canker sore to develop.
2. Localized Irritation: Some dental materials used during procedures may cause localized irritation to the soft tissues in the mouth. For instance, certain dental adhesives or filling materials can have an acidic or irritating effect on oral tissues, triggering the formation of canker sores. It’s crucial to note that each individual’s response to these substances may vary, as some people may be more prone to developing canker sores than others.

4. Possible Causes: Exploring the Factors Leading to Canker Sores after Dental Treatments
Canker sores are a common occurrence for many individuals after dental treatments. These painful ulcers can make it difficult to eat and speak comfortably, hindering day-to-day activities. While the exact cause of canker sores is still not completely understood, researchers have identified several potential factors that may contribute to their development. Exploring these causes can help both dental professionals and patients better understand and manage canker sores.
Possible causes of canker sores after dental treatments include:
- Oral Trauma: Accidental biting, aggressive brushing, or sharp dental instruments during treatments can lead to irritations and small tissue injuries that pave the way for canker sore formation.
- Certain Foods: Consuming acidic or spicy foods in the immediate post-treatment period can potentially trigger canker sores or exacerbate existing ones. Citrus fruits, tomatoes, and hot peppers are examples of such foods.
- Allergic Reactions: Some individuals may be sensitive or allergic to certain dental materials used during treatments, such as metals or adhesives. Allergic reactions can manifest as canker sores in the oral cavity.
- Stress and Hormonal Changes: Psychological stress, hormonal fluctuations, or lack of sleep can weaken the immune system, making individuals more susceptible to canker sores post-dental treatments.
It is important to note that these factors may not apply to everyone, and each individual’s experience can vary. Consulting with a dental professional is advised to determine the underlying cause of canker sores and develop an appropriate treatment plan for effective relief.
5. Prevention is Key: How to Minimize the Occurrence of Canker Sores Post-Dental Work
While canker sores can be quite bothersome and uncomfortable, there are steps you can take to minimize their occurrence after dental work. By following a few simple guidelines, you can promote faster healing and reduce the chances of developing canker sores. Here are some tips to keep in mind:
- Maintain good oral hygiene: Brush your teeth gently twice a day and floss daily to keep your mouth clean and free from harmful bacteria. This will help prevent any irritation or infection that could lead to canker sores.
- Avoid spicy or acidic foods: These types of foods can irritate the delicate tissues in your mouth, increasing the likelihood of canker sore formation. Opt for a soft and non-acidic diet during the healing period.
- Manage stress levels: Stress has been linked to canker sore outbreaks. Engage in stress-reducing activities like exercise, meditation, or hobbies that help you relax. Taking care of your mental well-being can have a positive impact on your overall oral health.
Remember, prevention is always better than cure when it comes to canker sores. By following these preventive measures, you can significantly reduce the chances of developing these painful ulcers post-dental work, allowing you to focus on a swift recovery and a healthy smile.
6. Managing the Discomfort: Tips and Remedies for Soothing Post-Treatment Canker Sores
Dealing with the discomfort of post-treatment canker sores can be a challenging experience. Thankfully, there are several tips and remedies you can try to soothe the pain and promote faster healing. Here are some helpful suggestions:
- Rinse with salt water: Mix half a teaspoon of salt in a glass of warm water and use it as a mouthwash. Rinse your mouth with this solution at least four times a day to help reduce inflammation and relieve pain.
- Apply a baking soda paste: Make a paste by combining a small amount of baking soda with a few drops of water. Apply this paste directly onto the canker sore, leave it on for a few minutes, and then rinse your mouth. Baking soda can help alleviate pain and facilitate healing.
- Use over-the-counter numbing gels: There are various gels available specifically formulated to numb the pain caused by canker sores. Apply a small amount onto the affected area to temporarily relieve discomfort.
Remember to avoid certain foods and drinks that can irritate the canker sores, such as spicy or acidic foods, citrus fruits, and carbonated drinks. Additionally, maintaining good oral hygiene by regularly brushing your teeth and using a soft-bristled toothbrush can help prevent further irritation. If the pain persists or the sore doesn’t improve after two weeks, it’s advisable to consult your healthcare professional for further guidance.
7. When to Seek Professional Help: Identifying when Canker Sores Require Dental Attention
When dealing with canker sores, it’s important to know when it’s necessary to seek professional dental help. While most canker sores heal on their own within 1-2 weeks, there are certain situations where dental attention is required. Here are some signs that indicate it’s time to consult a dentist:
- Severe pain: If the pain caused by the canker sore becomes unbearable and over-the-counter treatments aren’t providing relief, it may be time to see a dentist.
- Large or recurring sores: If the canker sore is unusually large, lasts longer than 2 weeks, or frequently reoccurs in the same location, it’s important to have it examined by a dental professional.
- Difficulty eating or speaking: Canker sores that interfere with your ability to eat, drink, or speak comfortably should be evaluated by a dentist to identify potential underlying causes.
Furthermore, if you experience other symptoms alongside canker sores, such as fever, swollen lymph nodes, or excessive drooling, it’s recommended to seek professional help. A dentist will be able to evaluate your condition accurately and provide appropriate treatments to alleviate the discomfort caused by canker sores.
8. Debunking Myths: Common Misconceptions about Post-Dental Work Canker Sores
Don’t let common misconceptions about post-dental work canker sores confuse you anymore! We’re here to debunk some of those myths and set the record straight. So, let’s address these misconceptions head-on:
Myth 1: Dental work causes canker sores.
- Fact: Contrary to popular belief, canker sores aren’t caused by dental procedures themselves.
- They may occur due to prolonged irritation from dental tools, cheek biting, or even increased stress during the treatment.
- It’s important to note that canker sores can also arise independent of any dental work, caused by factors like certain food sensitivities, viral infections, or hormone fluctuations.
Myth 2: Canker sores are contagious.
- Fact: You can breathe a sigh of relief – canker sores are not contagious!
- Unlike cold sores, which are caused by the herpes simplex virus and can be easily transmitted, canker sores are not caused by viruses.
- They are purely localized irritations that develop on the inside of the mouth and cannot be passed on to others through contact.
Now that you have a clearer understanding, it’s essential to separate fact from fiction when it comes to post-dental work canker sores. Remember, if you experience persistent discomfort or have concerns, it’s always best to consult with your dentist for personalized advice and proper diagnosis.
9. Long-Term Effects: Understanding the Outlook for Individuals with a History of Dental-Related Canker Sores
Individuals who have a history of dental-related canker sores may experience some long-term effects. While these effects vary from person to person, it is important to understand and be prepared for what they might be. Here are some key points to consider:
1. Increased susceptibility to canker sores: Having a history of dental-related canker sores may make you more prone to experiencing them in the future. Certain factors, such as stress, hormonal changes, or injury to the mouth, can trigger their recurrence. However, implementing good oral hygiene practices and following your dentist’s recommendations can help minimize their occurrence.
2. Impact on oral health: Canker sores can affect not only your comfort but also your overall oral health. Chronic or severe canker sores may interfere with eating, drinking, and speaking, leading to discomfort and difficulty performing daily activities. Additionally, if left untreated, canker sores can increase the risk of bacterial infections.
10. Conclusion: Empowering Patients with Knowledge to Navigate Post-Dental Work Canker Sores
In conclusion, arming yourself with knowledge on how to navigate post-dental work canker sores is crucial in empowering patients to effectively manage discomfort and promote quick healing. By implementing a few simple strategies, you can take control of your oral health and minimize the impact of canker sores:
1. Proper Oral Hygiene: Maintaining a good oral hygiene routine , including brushing your teeth twice a day, flossing daily, and using an antimicrobial mouthwash, can help prevent canker sores and support healing after dental procedures.
2. Avoiding Trigger Foods: Certain foods, such as citrus fruits, spicy foods, and sharp-edged snacks, can aggravate canker sores. Limiting your intake of these trigger foods can help prevent additional discomfort and speed up the healing process.
Frequently Asked Questions
Q: What are post-dental work canker sores? A: Post-dental work canker sores, also known as aphthous ulcers, are small, painful sores that can develop in your mouth after undergoing dental procedures or treatments.
Q: What causes canker sores after dental work? A: The exact cause is unknown, but several factors can contribute to the development of canker sores, such as trauma to the mouth tissues during dental work, stress, a weakened immune system, or certain nutritional deficiencies.
Q: How long do these canker sores typically last? A: In most cases, post-dental work canker sores heal on their own within 1-2 weeks. However, the healing time may vary for each individual.
Q: Are these canker sores contagious? A: No, post-dental work canker sores are not contagious. They are not caused by a virus or bacteria, so you don’t have to worry about spreading them to others.
Q: What are the common symptoms of post-dental work canker sores? A: Symptoms can include a burning or tingling sensation at the site, a round or oval-shaped sore with a white or yellowish center and a red border, pain or discomfort while talking, eating, or brushing teeth, and swollen lymph nodes in severe cases.
Q: How can I alleviate the pain and discomfort caused by these canker sores? A: You can try rinsing your mouth with a saltwater solution or over-the-counter mouthwash to help reduce pain and promote healing. Avoiding spicy or acidic foods, using a soft-bristled toothbrush, and practicing good oral hygiene can also aid in alleviating the discomfort.
Q: Should I seek treatment from a dentist for my post-dental work canker sores? A: In most cases, canker sores heal on their own and do not require any specific treatment. However, if the sores persist for more than two weeks, become extremely painful, or if you have recurrent canker sores, it’s advisable to consult your dentist for further evaluation and appropriate treatment options.
Q: Are there any preventive measures to avoid post-dental work canker sores? A: While canker sores cannot always be prevented, there are steps you can take to reduce the risk. These include managing stress levels, maintaining a balanced diet with adequate vitamins and minerals, practicing good oral hygiene, and informing your dentist about any history of canker sores before undergoing dental procedures.
Q: Can using certain dental products or medications trigger these canker sores? A: Some individuals may experience sensitivity or irritation from certain dental products like toothpaste or mouthwash that contain sodium lauryl sulfate (SLS). If you suspect this might be the case, you can try switching to SLS-free products to see if it helps. Additionally, some medications can also contribute to the development of canker sores, so it’s important to inform your dentist or doctor about any medications you are currently taking.
Q: How long does it take for the canker sores to completely heal? A: The healing time can vary for each individual. Generally, post-dental work canker sores take about 1-2 weeks to heal completely, but it’s not uncommon for them to take longer in some cases.
Remember, if you have any concerns or questions about post-dental work canker sores, it’s always best to consult with your dentist for professional advice tailored to your specific situation.
In conclusion, we hope that this article has shed some light on the perplexing issue of post-dental work canker sores. While these ulcers may be a bothersome aftermath of dental procedures, it is important not to panic or jump to conclusions. Remember, they are a fairly common occurrence and usually resolve on their own within a week or two.
By understanding the root causes and preventative measures, you can take proactive steps to minimize their occurrence and alleviate any discomfort. Remember, maintaining good oral hygiene, avoiding trigger foods, and practicing stress management techniques can go a long way in preventing these pesky canker sores.
Furthermore, if you do find yourself experiencing persistent or severe canker sores, don’t hesitate to reach out to your dentist or healthcare provider. They will be able to provide you with the necessary guidance and treatment options to ensure your comfort and peace of mind.
In the end, knowledge truly is power when it comes to uncovering the truth about post-dental work canker sores. Armed with this newfound understanding, you can approach your next dental procedure with confidence, knowing that any transient ulcers that may arise are nothing more than a minor inconvenience. So, keep that smile shining bright and embrace your journey towards optimal oral health!
Similar Posts

When to Ditch Gauze: Guide to Post-Wisdom Teeth Care!

Unveiling the Power of Lysine: Your Ally Against Canker Sores

Sushi After Wisdom Teeth Removal: When Can You Safely Indulge?

Unveiling Toothpaste Triggers for Canker Sores: Your Friendly Guide!

Post-Wisdom Teeth Removal: Can I Safely Take Advil?

Post-Wisdom Teeth Removal: Benefits of Using a Water Flosser!
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- All Wellness
- All Skin Care
- Moisturizers
- Mineral Sunscreens
- Sunscreens for Kids
- Sunscreens for Dark Skin
- SPF Lip Balms
- Under Eye Patches
- All Hair Care
- Purple Shampoos
- Thinning Hair
- Head Shavers
- Hair Dryers
- All Oral Care
- Electric Toothbrushes
- Toothpastes
- Mouthwashes
- Water Flossers
- Meal Kit Delivery
- Gluten-Free Meal Kit Delivery
- Disposable Face Masks
- Air Purifiers
- Eco-Friendly Laundry Detergents
- Natural Deodorants
- Period Underwear
- All Fitness
- Exercise Bikes
- Walking Shoes
- Fitness Trackers
- Reusable Water Bottles
- Blackout Curtains
- Sound Machines
- Home & Kitchen
- All Home & Kitchen
- Kitchen Appliances & Tools
- All Kitchen Appliances & Tools
- Coffee Makers
- Kitchen Gadgets
- Small Home Appliances
- All Small Home Appliances
- Air Conditioners
- Space Heaters
- Humidifiers
- Bedding & Bath
- All Bedding & Bath
- Bath Towels
- Silk Pillowcases
- Duvet Inserts
- Office Chairs
- Standing Desks
- Desk Organizers
- Seat Cushions
- Under Desk Ellipticals
- All Outdoor
- Raised Garden Boxes
- Garden Hoses
- Beach Towels
- Solar Pool Covers
- Grilling Accessories
- Electronics
- All Electronics
- Wifi Routers
- Gaming Consoles
- Streaming Devices
- Instant Cameras
- Handheld Gaming Consoles
- 3D Printers
- All Headphones
- Noise Canceling
- Wireless Earbuds
- Smart Gadgets
- All Smart Gadgets
- Smart Watches
- Smart Bulbs
- Garage Door Openers
- All Computers
- Gaming Laptops
- Laptops for College Students
- Computer Monitors
- Ergonomic Keyboards
- Dog Carriers
- Litter Boxes
- Scratching Posts
- Cat Carriers
- All Pet Care
- Nail Clippers
- Flea & Tick
- All Luggage
- Lightweight
- Weekender Bags
- Accessories
- All Accessories
- Luggage Tags
- Travel Pillows
- Tech Gadgets
- Packing & Organization
- All Packing & Organization
- Packing Cubes
- Toiletry Bags
- Gift Guides
- All Gift Guides
- Valentine's Day
- All Valentine's Day
- For Any Loved Ones
- Mother's Day
- All Mother's Day
- Last Minute Gifts
- Best Mother's Day Gifts
- For Moms Who Have Everything
- Best from Amazon
- All Graduation
- For College Grads
- For High School Grads
- For Teachers
- Father's Day
- All Father's Day
- Best Father's Day Gifts
- For Dads Who Love Fishing
- Holiday Season & Christmas
- All Holiday Season & Christmas
- Gifts Under $25
- Practical Gifts
- Other occasions & loved ones
- All Other occasions & loved ones
- For Grandparents
- For Bridal Shower
- For New Parents
- For Any Occasion
- Deals & Sales
- All Deals & Sales
- Most Popular This Month
- Sales This Week
- New & Notable
- What to Buy This Month
- All Sleep Week
- Body Pillows
- Sleep Week Sales
- Best of Wellness Awards 2024
- All Best of Wellness Awards 2024
- Winners as seen on TODAY
- View all of the winners here
- Winners on Amazon
- CNBC Select
- All CNBC Select
- Credit Cards
- Small Business
- Personal Finance
- Credit Monitoring
- Help for Low Credit Scores
- Sign up for the Select Newsletter
- Check out Shop TODAY
- Privacy Policy
- Do Not Sell My Personal Information
- Terms Of Service
- NBC News Sitemap
Follow Select
How to treat and prevent blisters, according to dermatologists and podiatrists

Everything about blisters is inconvenient. They’re unsightly, often painful and can prevent you from wearing your favorite pair of shoes or comfortably holding a dumbbell . But resist the temptation to pop or pick — proper care prevents infection and speeds up recovery. We spoke to dermatologists and podiatrists about how to treat blisters and prevent them in the first place. Using their expert guidance, we rounded up over-the-counter products to help you do both from brands like Neosporin, Band-Aid, Vaseline and more.
SKIP AHEAD How to treat blisters | The best blister treatments | How to prevent blisters | The best products to prevent blisters
Selected. Our top picks

select Is there actually a difference between foot cream and regular body moisturizer? We asked experts
How to treat blisters.
First things first — if you have a blister, stop doing whatever initially caused it, says Dr. Stephanie Saxton-Daniels , a board-certified dermatologist at Westlake Dermatology in Dallas, Texas. That may mean not wearing a certain pair of shoes or taking a break from lifting weights. If you continue applying friction to the affected area, the blister will likely get worse or even pop, which is painful and can lead to an infection.
There are three main steps you should follow to treat a blister. Each one requires different over-the-counter products.
- Gently wash the affected area : Use warm water and a mild, fragrance-free soap, and then pat dry. Don’t press or rub too hard while washing the affected area, and clean your hands before you begin.
- Apply a topical antibacterial or occlusive ointment : Regardless of what over-the-counter product you use, choose something made without irritants like fragrances, artificial scents or alcohols, experts told us. Antibacterial ointments contain ingredients that the skin absorbs to slow down or stop bacteria growth, thus preventing infections. Occlusive ointments create a physical barrier on top of skin, keeping it moist and hydrated.
- Cover the blister with a bandage : Place a fabric or hydrocolloid bandage over the blister to reduce discomfort, swelling and irritation, says Saxton-Daniels. Try to buy a box that comes with at least 14 bandages since blisters can take a week or two to heal, and you’ll need to change the bandage at least once a day, says Dr. Maryann Hartzell, the medical director of the Foot and Ankle Institute at Temple University’s School of Podiatric Medicine.
The best blister treatments
Aveeno skin relief fragrance-free body wash.

Aveeno makes some of our favorite body washes for sensitive skin , and this one is ideal for cleansing the area around your blister since it’s fragrance-free and dye-free. It’s formulated with moisturizing ingredients like oat flour, extract and oil. The liquid body wash turns into a rich, creamy lather as you use it.
Vaseline Original Healing Jelly

Applying an occlusive ointment to blisters can help reduce friction when the area rubs up against clothing or shoes, says Dr. Mary Stevenson , a dermatologic surgeon and an associate professor of dermatology at NYU Langone Health. Vaseline, which is made from 100% petroleum jelly, is one option that’s beloved by many NBC Select staffers. You can use it on blisters, sunburns , dry skin and chapped lips , so it’s worth keeping a jar at home. Vaseline earned the National Eczema Association’s Seal of Acceptance, and it’s fragrance-free, hypoallergenic and won’t clog pores, according to the brand.
Neosporin Original Antibiotic Ointment

While you should not purposely pop a blister, they can pop on their own. In these cases, applying an antibiotic ointment is important to prevent bacteria from getting inside the open wound, experts told us. Neosporin is a topical antibiotic ointment many NBC Select staffers have used for years, and it’s made with bacitracin zinc, neomycin sulfate and polymyxin B, ingredients that help prevent skin infections, according to the brand. You can apply a small amount to your blister up to three times a day until the wound closes.
Band-Aid Flexible Fabric Bandages

You don’t have to cover a closed blister, but doing so often makes people more comfortable, especially if they have a blister somewhere that experiences consistent friction, like the feet when they’re in shoes, says Saxton-Daniels. Covering a popped blister, however, is a must — doing so prevents dirt and germs from getting inside the open wound. Bandages like these have adhesive on both sides to stick to skin and a piece of gauze in the middle to cushion and protect the blister. Band-Aids are flexible so they move with you and stay on for up to 24 hours, according to the brand. This pack comes with Band-Aids in different sizes so you can choose the one that best fits your blister. Many NBC Select staffers keep Band-Aids in their at-home first aid kits since they frequently come in handy.
All Health Advanced Fast Healing Hydrocolloid Gel Bandages

All Health Hydrocolloid Gel Bandages
Stevenson recommends using bandages made from hydrocolloid, an occlusive dressing, to cover blisters. Hydrocolloid bandages are made with an ingredient that turns into a gel when it absorbs fluids, creating a moist environment that encourages healing, according to the brand. The bandages also form a seal around the affected area you’re covering, keeping dirt, germs and water out. Since these bandages are soft, they won’t stick to or pull on your blister. They stay on for up to seven days, but our experts recommend replacing your bandage daily. For best results, the brand recommends applying the bandages, which have a 4.5-star average rating from 23,424 reviews on Amazon, on totally dry skin. So if you use an ointment beforehand, wait a bit before placing the hydrocolloid bandage on top.

select Can’t get rid of your rough, dry feet? This at-home treatment could help.
How to prevent blisters.
Preventing most blisters involves eliminating friction between a surface, like the heel of your sneaker or the handle of a gardening tool , and your skin. You can do so by padding an area on your body with a bandage or lubricating the skin with something like an anti-chafing stick .
Wearing protective clothing like socks and gloves can also prevent blisters, says Saxton-Daniels. And as far as the feet are concerned, avoid walking barefoot on hot surfaces, like pavement in the warmer months, and be sure to wear properly fitting shoes at all times, says Dr. Jacob Wynes , a podiatric surgeon and an associate professor of foot and ankle surgery for the University of Maryland Medical System. Shoes shouldn’t feel so tight that they’re restrictive, or like your feet are sliding around in them, he says.
The best products to prevent blisters
Dr. scholl’s moleskin padding roll.

Moleskin is a woven cotton fabric, and Saxton-Daniels recommends using bandages made from the material to pad areas that may experience frequent friction, like certain parts of the feet depending on what shoes you’re wearing. The bandage prevents the skin from making direct contact with whatever is rubbing up against it, reducing potential irritation and discomfort, she says. Dr. Scholl’s moleskin padding comes in a roll, allowing you to customize the size of each piece you cut, and it has a skin-safe adhesive on the back. The bandage, which has a 4.6-star average rating from 10,932 reviews on Amazon, is thin enough that it won’t impact how your shoes fit, according to the brand.
Nexcare Blister Prevention Tape

Nexcare’s Blister Prevention Tape is made from flexible, cushioned foam that has water-resistant, skin-safe adhesive on the back, helping it stay on your body even while you’re sweating, according to the brand. The tape, which is one inch wide, comes in a roll so you can customize the size of each piece you cut or wrap it around your hands, fingers, feet or ankles. It has a 4.6-star average rating from 20,543 reviews on Amazon.
Foot Petals Spot Dot Cushion

I always keep these little cushions at home because they’re quick fixes for shoes that are irritating my feet. I place them inside my shoes in areas that are rubbing against my skin and could lead to a blister if I wasn’t proactive. The cushions are about one-inch by one-inch large and have an adhesive back, helping them stick to the interior of shoes. They don’t start to lose their stickiness over time, in my experience — I put a few cushions in a pair of winter boots and they’ve stayed put for over two years. I also frequently cut the cushions in half so they fit smaller areas in my shoes, like a thick strap on a sandal.
Body Glide Foot Glide

Before wearing shoes without socks, like sandals, slides or flip flops, you can apply this clear balm to your feet to prevent straps and buckles from rubbing on your skin. It’s made from plant wax, which is water-resistant, sweat-resistant and fragrance-free, plus it doesn’t have a greasy or oily feel. It has a 4.5-star average rating from 12,819 reviews on Amazon.
Topsome Shoe Stretcher

In addition to wearing socks when it makes sense, it’s important that your shoes fit well and are broken-in before wearing them for extended periods of time, says Hartzell. If you try shoes on and are worried that they’re a bit too tight, consider stretching them out with a shoe stretcher like this one. You can use it to make shoes wider and longer, as well as add space above the top of the foot. The shoe stretcher, which has a 4.5-star average rating from 5,142 reviews on Amazon, comes with eight bunion plugs, allowing you to stretch whatever specific area your bunion rubs up against.
Frequently asked questions
Blisters are fluid-filled sacs that form underneath the skin’s surface, says Hartzell. They’re usually caused by something repeatedly rubbing against and creating friction with your skin, like a pair of shoes. You can get blisters anywhere on the body, but they most commonly occur on the feet and hands, she says.
There are three main types of blisters: friction blisters, blood blisters and heat blisters. Blisters can also form due to allergic reactions or certain skin conditions, which you’d need to see a doctor about.
Friction blisters
Friction blisters are the most common type. They’re caused by repeated rubbing or friction, and they form when clear liquid builds up under the upper layers of the skin, says Hartzell. Many people get friction blisters on their feet if they wear ill-fitting shoes for extended periods of time or if they don’t wear socks. But you can also get friction blisters on your hands from holding tools or gym equipment. Speaking from personal experience, kids are prone to friction blisters on their hands if they frequently use the monkey bars on the playground.
Blood blisters
Blood blisters usually form after something pinches your skin — for example, if part of your hands or fingers gets caught between the heads of pliers or gardening pruners. Instead of clear liquid, blood from broken vessels builds up under the skin to form a blister, says Hartzell.
Heat blisters
Burns and sunburns can blister, and if they do, they’re classified as second-degree burns, says Hartzell. Blisters may also form as someone warms up while recovering from frostbite.
Blisters can last days or weeks, depending on how large the blister is and where it’s located, says Stevenson. Eventually, your body reabsorbs the fluid that’s inside the blister and it goes away. But if it feels like your blister isn't getting better despite consistent treatment, experts recommend consulting your doctor.
No, you should not pop a blister or remove the roof of a blister (meaning the skin that covers it), says Saxton-Daniels. The fluid inside a blister serves as protective dressing over healing skin and prevents the deeper layers of skin from developing an infection.
Most people don’t need to see a doctor about a blister, but if you experience any of the following symptoms, experts say it’s a good idea to consult a medical professional.
- If you frequently develop blisters in areas where there is no friction, and cannot identify the cause of them.
- If your blister does not resolve within a week or two, or is getting worse despite consistent treatment.
- If your blister is larger than two to three inches in size.
- If your blister appears infected. Signs of infection include red, swollen, hot, painful skin surrounding the blister; a blister filled with a white or yellow-ish liquid rather than clear fluid or blood; yellow-ish or green-ish discharge; and red streaks around the blister.
Meet our experts
At NBC Select, we work with experts who have specialized knowledge and authority based on relevant training and/or experience. We also take steps to ensure that all expert advice and recommendations are made independently and with no undisclosed financial conflicts of interest.
- Dr. Stephanie Saxton-Daniels is a board-certified dermatologist at Westlake Dermatology in Dallas, Texas.
- Dr. Mary Stevenson is a dermatologic surgeon and an associate professor of dermatology at NYU Langone Health.
- Dr. Maryann Hartzell is the medical director of the Foot and Ankle Institute at Temple University’s School of Podiatric Medicine.
- Dr. Jacob Wynes is a podiatric surgeon and an associate professor of foot and ankle surgery for the University of Maryland Medical System.
Why trust NBC Select?
Zoe Malin is an associate updates editor at NBC Select who writes about skin care, including stories on how to treat ingrown hairs , sunburns and razor burn . For this article, she interviewed three experts about how to treat blisters and rounded up the best products to do so with their guidance in mind.
Catch up on NBC Select’s in-depth coverage of personal finance , tech and tools , wellness and more, and follow us on Facebook , Instagram , Twitter and TikTok to stay up to date.
Zoe Malin is an associate updates editor for Select on NBC News.

IMAGES
VIDEO
COMMENTS
If you've ever cancelled a dental appointment, it was probably because of something like a flat tire, the school calling you about your child being sick, or losing your dental insurance.It probably wasn't because of a cold sore. But guess what, your cold sore — or fever blister — is highly contagious. It may not seem like that much of a big deal, but it can pose some serious issues ...
Fever Blisters (also known as cold sores) are painful fluid-filled sores that form on the outside of the mouth around the lips. Fever blisters are very contagious. Canker Sores are painful white or yellow sores that only form inside the mouth, usually on the insides of the cheeks or lips or on the tongue. Canker sores (also called aphthous ...
A cold sore is a blister that typically appears on your lip or around your mouth. The herpes simplex virus type 1 (HSV-1) causes most cold sores. HSV-1 is very contagious. You can prevent getting cold sores by avoiding kissing people with them or sharing objects with them. Cold sores usually go away on their own within a couple of weeks.
Cold sores, or fever blisters, are a common viral infection. They are tiny, fluid-filled blisters on and around the lips. These blisters are often grouped together in patches. After the blisters break, a scab forms that can last several days. Cold sores usually heal in 2 to 3 weeks without leaving a scar.
Stage 4: Crusting. Like other wounds, after cold sore blisters rupture, they crust and form scabs. Crusting and scabbing typically occur 4 to 5 days after cold sores appear. Scabs may crack or bleed a bit as they heal. Do not try to pick or pull off scabs or crusting.
Some dentists, however, will begin seeing people with cold sores again after that healing process has started and the sores have begun to scab. Even after that point, some people may experience pain from the dried-out sores. It might be hard to keep your mouth open for extended periods. This is perfectly normal and your dentist would understand ...
Key points. Cold sores are small blisters around the mouth, caused by the herpes simplex virus. Cold sores can be spread by kissing or sharing eating utensils or even sharing towels. Tingling often occurs prior to the appearance of blisters. Cold sores cause small blisters on the lips and mouth that enlarge, burst, then crust over.
FACT SHEET: Herpes Simplex Infection (various intra- or peri-oral infections/manifestations also known as herpetic gingivostomatitis, herpes labialis, herpes simplex labialis, oral herpes, cold sore, and fever blister; finger infection known as herpetic whitlow; caused by herpes simplex virus type 1 [HSV-1] and less commonly by herpes simplex virus type 2 [HSV-2])
Cold sores happen in stages: You have a tingling, burning, or itching feeling. About 12-24 hours later, blisters form. The area becomes red, swollen, and painful. The blisters break open and fluid ...
Cold sores are groups of painful, fluid-filled blisters (often called "fever blisters"). These unsightly sores usually erupt on the lips, and sometimes on skin around the lips. Clusters of small blisters also may occur on the gum tissue near the teeth and/or on the bony roof of the mouth. Cold sores are caused by herpesvirus Type 1 or Type ...
Cold sores, also known as fever blisters, are caused by the herpes simplex virus type one (HSV-1). The virus lives in your nerves but damages your skin. It causes sores around the face, usually the lips, that last about one week. In rare cases, cold sores can appear on other parts of your body. The virus spreads easily by coming in contact with ...
Overview. Cold sores and fever blisters are caused by herpes simplex virus type 1 (HSV-1). This virus is passed from person to person by saliva (either directly, or by drinking from the same glass or cup) or by skin contact. Cold sores usually appear as clusters of tiny blisters on the lip. About 8 out of 10 people have the virus that causes ...
The United States Centers for Disease Control and Prevention (CDC) does not give specific guidance related to treating patients with cold sores. However, the CDC recommends work restrictions for clinicians with active herpes lesions on the hands (herpetic whitlow) to avoid patient contact until the lesions heal. 4.
Eat healthy food and make sure to take your daily dose of vitamin C in the days leading up to your appointment. 2. Ask your doctor for antiviral medicines. Speak with your trusted doctor to tell them about your cold sore situation that happens every time you visit the dentist.
If you experience canker sores after dental treatment, here are a few things that you can do to help relieve the pain and speed healing: Apply ice or a cold pack to the sore for 10-15 minutes daily. This will help reduce inflammation and pain. Take over-the-counter pain medications such as ibuprofen or acetaminophen to help relieve pain.
These symptoms can include a fever, chills, fatigue, and aches and pains throughout the body. While it is not common, it is vital to be aware of the potential side effects of dental work so you can take the necessary steps to alleviate any discomfort or symptoms that may arise. If you experience these symptoms after a visit to the dentist, be ...
The virus can lie dormant in the nerve tissue of the face. When the virus is reactivated, it can cause outbreaks. Despite it's prevalence, many people never experience symptoms or outbreaks. However, this means they could infect others unwittingly, or experience an unexpected outbreak following a trauma like dental work.
Use good quality sunscreen on your lips. Avoid stress whenever possible. And ask your dentist about antiviral medicines that can prevent sores from developing. Certain medicines that help fever blisters to heal faster may also help to prevent them from forming in the first place, including acyclovir (Zovirax), famciclovir (Famvir), and ...
Cold sores (fever blisters) appear on the outside of your mouth, often on your lips. A virus causes them, and they're very contagious. If you have a fever blister, you should avoid sharing personal items with other people to reduce the spreading of the virus. ... Visit your dentist regularly for checkups and cleanings. If your provider thinks ...
Fever Blisters After Treatment. Occasionally, within a few days after children receive dental treatment, groups or clusters of painful blisters or sores may occur on or around the lips. These sores, often called cold sores or fever blisters, may first appear as reddish areas and can progress to ulcers quickly. The sores can be very painful.
Cold sores and fever blisters are caused by herpes simplex virus type 1 (HSV-1). This virus is passed from person to person by saliva (either directly, or by drinking from the same glass or cup) or by skin contact. Cold sores usually appear as clusters of tiny blisters on the lip. About 8 out of 10 people have the virus that causes cold sores.
A cold sore, also known as herpes labialis or a fever blister, is a harmless but irritating fluid-filled blister that goes away in about 10 days from the first symptom (tingling or burning sensation). They appear on the lips and sometimes the skin around the lips. Herpes labialis, a cold sore virus, is contracted like any other virus.
Trauma: Dental procedures can cause minor injury or irritation to the delicate tissues in your mouth, leading to the formation of canker sores. Bacterial infections: Occasionally, various bacteria present in the oral cavity can invade the damaged tissue, increasing the risk of canker sore development. Allergies or chemical irritants: Some individuals may have a sensitivity or allergic reaction ...
There are three main steps you should follow to treat a blister. Each one requires different over-the-counter products. Gently wash the affected area: Use warm water and a mild, fragrance-free ...